
Visualized bilateral breast reconstruction by propeller thoracodorsal artery perforator flaps
Introduction
The thoracodorsal artery perforator (TAP) flap has been widely used for breast reconstruction since it was first described by Angrigiani et al. (1) in 1995. The TAP flap is an alternative to the more established muscular latissimus dorsi (LD) flap (2,3). The LD flap has, however, shown an accumulation of donor-site morbidity such as chronic pain, seroma formation and reduced shoulder function (4-6). Due to this morbidity the TAP flap has gained foothold in breast reconstruction (7,8).
Since the first presentation of the TAP flap it has been further developed to accommodate the demands in breast reconstruction. The flap can be used as a pedicled perforator flap or a propeller flap and can be used with or without implants (9,10). In 2008 Hamdi et al. shared their experience of implant assisted TAP flaps and discussed the risk of blood flow restriction (11).
The TAP flap is an alternative to the LD flap and in cases, where a deep inferior epigastric artery (DIEP) is impossible or contraindicated. We have previously described our unilateral and bilateral methods for TAP flap breast reconstruction (5,12-14). In this visualized surgery paper, we aim to show and describe how we perform bilateral propeller TAP flap breast reconstruction and share our results using this technique.
Material and methods
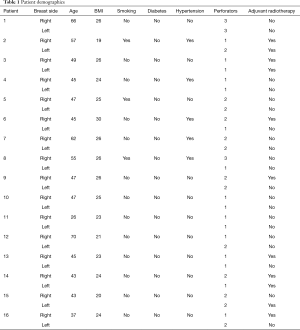
We retrospectively collected data on 16 women having a bilateral propeller TAP flap breast reconstruction. We recorded major complications, type of implants, total operating time and follow-up in days.
Patient selection
Patient selection is essential for a successful outcome. In our practice all patients eligible for a delayed breast reconstruction are informed comprehensively about advantages and disadvantages of the different reconstructive methods. We inform about the LD flap, the TAP flap, the DIEP flap, the profunda artery perforator (PAP) flap or transverse/vertical musculocutaneous gracilis (TMG) flap. Patients with a low BMI and too little volume in the abdomen and thighs are candidates for a LD or a TAP flap breast reconstruction. Following information about the different reconstructive options, some patients do not want a free flap breast reconstruction and choose to be reconstructed with a pedicled flap from the back. The patients included in this study all choose a TAP flap breast reconstruction based on the comprehensive information about their reconstructive options. Factors in favour of TAP flaps in our practice include but are not limited to: post-mastectomy radiotherapy, excess scar tissue, skin not suitable for expansion, patient desire, and other patient factors discouraging or preventing free flap breast reconstruction. The study population consisted of 16 women aged 26–70 who had undergone bilateral mastectomy prior to the reconstruction. Patient demographics are presented in Table 1.
Full table
Preoperative drawings
Color Doppler ultrasonography (CDU) was used preoperatively in all patients to locate the thoracodorsal perforators. All of the patients except one had a one or two stage bilateral propeller TAP flap breast reconstruction. The last patient was reconstructed in a triple stage breast reconstruction due to small and fragile perforators identified by CDU. The patient had previously been treated by bilateral mastectomy. On the left side the patient had adjuvant radiation therapy and the pectoralis major muscle had been removed as part of the ablative procedure. The patient, a healthy 43-year-old, had a low BMI of 20. We evaluated if it was possible to reconstruct the breasts by free flaps but neither the DIEP flap nor the profunda artery perforator flap or transverse/vertical TMG flap would supply sufficient amounts of tissue for breast reconstruction, Figure 1. The one possibility would be stacked free flaps. We presented the possibilities to the patient and she chose a bilateral delayed breast reconstruction using propeller TAP flaps with implants.
Stage 1: raising the TAP flaps (Figure 2)

The video shows the planning and how we raised the flaps, raising the TAP flaps (Figure 2). Two perforators were identified and visualized on both sides by CDU and marked by permanent marker. We usually raise the TAP flap in a direction going from the distal medial tip towards the perforators. However, in this case we maintained a small attachment of subcutaneous tissue near the distal tip of the flap to facilitate the vascular delay procedure. The flap was raised entirely except the attachment around the perforators and the subcutis at the distal tip. The flap was sutured in one layer by Monocryl 3.0 running sutures and left in place as part of the delay procedure.
Stage 2: rotating the flap to the recipient site (Figure 3)

This video shows the second surgical procedure performed 14 days after the first procedure, rotating the TAP flaps (Figure 3). The evaluation preoperatively showed that both TAP flaps were vital and well-perfused in the entire surface (Figure 4). The markings for the second procedure were marked by permanent marker.
The patient was placed in the supine position on the operating table. The skin at the recipient sites at the anterior thorax was incised by scalpel at the level of the inframammary crease and the flaps were raised as fasciocutaneous flaps. Wet surgical towels were placed under the flaps and covered with transparent drape. The patient was then turned to the prone position and the TAP flaps were raised by blunt and some sharp dissection. The wet towels were identified and removed from the anterior pockets and the TAP flaps were rotated into the pockets. The donor sites were closed in three layers using PDS 0, Vicryl 2.0 and Monocryl 3.0 running sutures. The patient was then turned to the prone position and the TAP flaps were sutured to the recipient site using Vicryl 3.0 and Monocryl 3.0 sutures.
Stage 3: implant reconstruction (Figure 5)

This video shows the third stage of the propeller TAP flap breast reconstruction, breast reconstruction by implants (Figure 5). The breast was marked by permanent marker (Figure 6). The skin was incised by scalpel at the location of the inframammary crease and surgery commenced using monopolar cautery. The width and height of the breast base was measured and the implants, Mentor CPG 331, 380 cc were placed in a prepectoral pocket on both sides due to a thin pectoralis major muscle on the right side and a missing muscle on the left side. The tissue was sutured in three layers using Vicryl 3.0 and Monocryl 3.0 sutures.
Results
We achieved a total of 32 reconstructed breasts in 16 patients. Major complications requiring surgical intervention were seen in 5/32 (16%) breasts with necrosis at the tip of the flaps, less than 10% of the surface. Anatomical implants were chosen for direct to implant reconstruction in 24/32 (75%), two stage reconstruction with expanders in 6/32 (19%) and triple stage in 2/32 (6%) reconstructions. The mean implant size were 360 cc (range, 250–650 cc). The mean operating time for the first procedure was 260 minutes (range, 180–383 minutes) for the 13 patients having a one-stage direct to implant and the two patients having a two-stage expander to implant TAP flap breast reconstructions. The mean follow-up was 627 days (range, 0–1,295 days). Results are presented in Table 2.
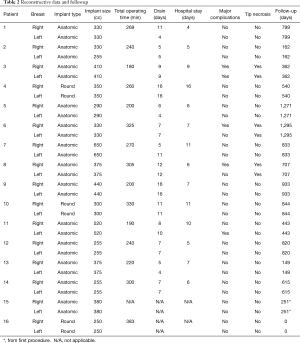
Full table
Discussion
We have successfully achieved 32 breast reconstructions in 16 women using propeller TAP flaps in combination with implants. The principles and technique are visualized in the three videos showing a case where we had to perform the procedure as a delay procedure. Our original plan was to perform the procedure in the video’s as a two-stage procedure. Raising the TAP flaps in the first stage, leave them in place as a delay procedure and then rotate the flaps and reconstruct with implants in the second stage. However, as we had turned the flaps in the second procedure, we deemed the perfusion of the flaps too poor for implant reconstruction and chose a triple stage procedure for safety. The videos show the three stages of breast reconstruction using propeller TAP flaps with implants for bilateral breast reconstruction. However, in the majority (94%) of cases, it was possible to perform the reconstruction in one stage or as a two-stage procedure.
The three steps in the one- and two-stage procedures are: (I) raise the flaps, either fasciocutaneous or musculocutaneous, at the recipient site and place a wet surgical towel under the flaps and cover with transparent drape with the patient placed in the supine position; (II) raise the TAP flaps and rotate the flaps to the recipient site in exchange of the wet towels with the patient in the prone position and (III) reconstruct the breasts with implants or expanders with the patient in the supine position.
We experienced five cases with major complications (all tip necrosis less than 10% of the flap surface) needing revision surgery in general anesthesia. These cases occurred in the beginning, when we started using the TAP flap for breast reconstruction and was a part of our learning curve using this technique. We have described this problem, which is associated to flap perfusion and angiosome distribution in the TAP flap (18). The blood supply of the most distal part and third angiosome of the TAP flap is variable (19-21). We have recently introduced ICG angiography and expect major complications to be reduced to a minimum in future patients.
Different alternatives in breast reconstruction exist and the chosen reconstructive method should take patient factors and wishes into account. The TAP flap is an alternative to other secondary reconstructive options, LD flaps and free flaps (14,22). The surgeon should guide the patient to select the best reconstructive option considering patient wishes, comorbidity and the available tissue and blood supply.
The TAP flap itself has several advantages. It seems to have lesser impact on shoulder function in comparison with the LD flap and can be used when free flaps or expansion are discouraged due to patient factors or wishes. Furthermore, it is more readily available for the general plastic surgeon and is a relatively fast option for bilateral breast reconstruction in comparison with free flap reconstruction (13,23,24).
CDU can be used not only to identify the perforators but can also be used as a tool in the surgical planning, drawing and dissection of the flap (5,18,25). The use of CDU may allow for faster dissection and thus decrease operating time. We inform all our TAP flap candidates that 75% of the breast reconstructions can be performed as a direct to implant procedure using a silicone implant and that 25% needs to a two-stage procedure using an expander-to-implant approach due to a poorer vascular supply (13).
Preoperatively, we use CDU to evaluate the size of the perforators to get an impression of the blood flow. We have performed more than 120 delayed TAP flap breast reconstructions, unilateral and bilateral, and with experience we now use the preoperative CDU to evaluate if a two-stage approach is needed based on the perforator size and flow. However, the use of CDU is subjective and observer dependent. We inform the patients, that the final decision about a one-stage or a two-stage is made during surgery, when the flap is raised and transposed.
The patient in the video were so skinny, that free flap breast reconstructions using tissue from the abdomen or thighs were not possible and furthermore the patient did not want free flap reconstructions following information about the options. The patient did not want bilateral LD breast reconstructions either. The CDU of the perforators revealed very gracile TAP perforators. Based on this knowledge, we choose the safest solution, a triple-stage procedure. The use of CDU can however be limited by the misconception that it is difficult to use, requiring much training and expertise. We started using TAP flaps for delayed breast reconstruction in 2011 due to a concern about shoulder morbidity and performed our first bilateral TAP flap breast reconstruction in 2011. There is a learning curve to the use of not only the TAP flap, but using pedicled perforator flaps for reconstruction in all areas of the body (5,12,14,22,23).
It is well-known that the boundaries of the angiosomes can be a challenge (18,25-28). However, with increasing experience, the use of CDU and lately ICG, the risk of major and minor complications have diminished to a minimum. All of the patients intended for a bilateral TAP flap breast reconstruction in this series ended up having successful bilateral breast reconstructions. In our experience, the success rate for TAP flap breast reconstructions is more than 98% and increasing (13).
Conclusions
The technique and principles of bilateral propeller TAP flap breast reconstruction with implants is visualized. The propeller TAP flap can be used for bilateral breast reconstruction as an alternative to other reconstructive options, when patient factors and wishes are favorable.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: The patient appearing in the videos have given informed consent to the use of the video footage.
References
- Angrigiani C, Grilli D, Siebert J. Latissimus dorsi musculocutaneous flap without muscle. Plast Reconstr Surg 1995;96:1608-14. [Crossref] [PubMed]
- Schneider WJ, Hill HL, Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. British Journal of Plastic Surgery 1977;30:277-81. [Crossref] [PubMed]
- Hammond DC. Latissimus dorsi flap breast reconstruction. Plast Reconstr Surg 2009;124:1055-63. [Crossref] [PubMed]
- Spear SL, Hess CL. A review of the biomechanical and functional changes in the shoulder following transfer of the latissimus dorsi muscles. Plast Reconstr Surg 2005;115:2070-3. [Crossref] [PubMed]
- Børsen-Koch M, Gunnarsson GL, Udesen A, et al. Direct delayed breast reconstruction with TAP flap, implant and acellular dermal matrix (TAPIA). J Plast Reconstr Aesthet Surg 2015;68:815-21. [Crossref] [PubMed]
- Adams WP Jr, Lipschitz AH, Ansari M, et al. Functional donor site morbidity following latissimus dorsi muscle flap transfer. Ann Plast Surg 2004;53:6-11. [Crossref] [PubMed]
- Hamdi M, Decorte T, Demuynck M, et al. Shoulder function after harvesting a thoracodorsal artery perforator flap. Plast Reconstr Surg 2008;122:1111-7. [Crossref] [PubMed]
- Rindom MB, Gunnarsson GL, Lautrup MD, et al. Shoulder-related donor site morbidity and patient-reported satisfaction after delayed breast reconstruction with pedicled flaps from the back: A comparative analysis. J Plast Reconstr Aesthet Surg 2018;71:1108-15. [Crossref] [PubMed]
- Hamdi M, Van Landuyt K, Hijjawi JB, et al. Surgical technique in pedicled thoracodorsal artery perforator flaps: a clinical experience with 99 patients. Plast Reconstr Surg 2008;121:1632-41. [Crossref] [PubMed]
- Angrigiani C, Rancati A, Escudero E, et al. Propeller thoracodorsal artery perforator flap for breast reconstruction. Gland Surg 2014;3:174-80. [PubMed]
- Hamdi M, Salgarello M, Barone-Adesi L, et al. Use of the thoracodorsal artery perforator (TDAP) flap with implant in breast reconstruction. Ann Plast Surg 2008;61:143-6. [Crossref] [PubMed]
- Gunnarsson GL, Børsen-Koch M, Nielsen HT, et al. Bilateral breast reconstruction with extended thoracodorsal artery perforator propeller flaps and implants. Plast Reconstr Surg Glob Open 2015;3:e435. [Crossref] [PubMed]
- Gunnarsson GL, Holm J, Duus N, et al. Propeller TAP flap breast reconstruction: A simplified surgical technique. J Plast Reconstr Aesthet Surg 2018;71:1424-31. [Crossref] [PubMed]
- Thomsen JB, Bille C, Wamberg P, et al. Propeller TAP flap: is it usable for breast reconstruction? J Plast Surg Hand Surg 2013;47:379-82. [Crossref] [PubMed]
- Lorenzen MM, Gunnarsson GL, Bille C, et al. Raising the TAP flaps. Asvide 2019;6:291. Available online: http://www.asvide.com/watch/32976
- Lorenzen MM, Gunnarsson GL, Bille C, et al. Rotating the TAP flaps. Asvide 2019;6:292. Available online: http://www.asvide.com/watch/32977
- Lorenzen MM, Gunnarsson GL, Bille C, et al. Breast reconstruction by implants. Asvide 2019;6:293. Available online: http://www.asvide.com/watch/32978
- Gunnarsson GL, Tei T, Thomsen JB. Color Doppler Ultrasonography-Targeted Perforator Mapping and Angiosome-Based Flap Reconstruction. Ann Plast Surg 2016;77:464-8. [Crossref] [PubMed]
- Alstrup T, Christensen BO, Damsgaard TE. ICG angiography in immediate and delayed autologous breast reconstructions: peroperative evaluation and postoperative outcomes. J Plast Surg Hand Surg 2018;52:307-11. [Crossref] [PubMed]
- Burnier P, Niddam J, Bosc R, et al. Indocyanine green applications in plastic surgery: a review of the literature. J Plast Reconstr Aesthet Surg 2017;70:814-27. [Crossref] [PubMed]
- Griffiths M, Chae MP, Rozen WM. Indocyanine green-based fluorescent angiography in breast reconstruction. Gland Surg 2016;5:133-49. [PubMed]
- Thomsen JB, Gunnarsson GL. The evolving breast reconstruction: from latissimus dorsi musculocutaneous flap to a propeller thoracodorsal fasciocutaneous flap. Gland Surg 2014;3:151-4. [PubMed]
- Jacobs J, Børsen-Koch M, Gunnarsson GL, et al. The versatile extended thoracodorsal artery perforator flap for breast reconstruction. Ann Plast Surg 2016;77:396-400. [Crossref] [PubMed]
- Ortiz CL, Mendoza MM, Sempere LN, et al. Versatility of the pedicled thoracodorsal artery perforator (TDAP) flap in soft tissue reconstruction. Ann Plast Surg 2007;58:315-20. [Crossref] [PubMed]
- Ibrahim RM, Gunnarsson GL, Akram J, et al. Color Doppler ultrasonography targeted reconstruction using pedicled perforator flaps—a systematic review and meta-analysis. Eur J Plast Surg 2018;41:495-504. [Crossref] [PubMed]
- Gunnarsson GL, Thomsen JB. The versatile modiolus perforator flap. Plast Reconstr Surg Glob Open 2016;4:e661. [Crossref] [PubMed]
- Gunnarsson GL, Jackson IT, Westvik TS, et al. The freestyle pedicle perforator flap: a new favorite for the reconstruction of moderate-sized defects of the torso and extremities. Eur J Plast Surg 2015;38:31-6. [Crossref] [PubMed]
- Gunnarsson GL, Jackson IT, Thomsen JB. Freestyle facial perforator flaps—a safe reconstructive option for moderate-sized facial defects. Eur J Plast Surg 2014;37:315-8. [Crossref] [PubMed]





