Visualized immediate breast reconstruction with dermal flap and implant
Introduction
Immediate implant based breast reconstruction has been used for more than 50 years (1), and skin-sparing as well as nipple-sparing direct-to-implant breast reconstruction has gained popularity over the last decade for both risk reducing and therapeutic cases (2,3). The use of biological and synthetic meshes has become a favored addition to immediate breast reconstruction (4,5). However, the extra cost of these meshes encourages surgeons to develop and refine the classic surgical techniques (6). Reconstructive methods are undergoing constant refinement, but treating women with large, ptotic breasts is still a surgical challenge. These women need reduction and reshaping of the skin envelope, and a higher nipple position for an optimal cosmetic result. Two-stage procedures are commonly used, either by removing skin and nipple with expander to implant reconstruction, or breast reduction prior to direct-to-implant reconstruction (7). Bostwick described the use of a dermal sling and implant for Wise pattern mastectomy and immediate expander prosthesis reconstruction in 1990, and a few modifications have been reported (6,8), however, this method is not yet widely used.
The aim of this paper is to visualize direct to implant immediate breast reconstruction using an inferior dermal flap.
Operative technique
The surgical technique is demonstrated in the video (Figure 1) “Immediate breast reconstruction with dermal flap and implant”.

Patient evaluation
Patients with large, ptotic breasts where the skin envelope is too large for a standard direct-to-implant reconstruction, may be eligible for dermal flap and implant reconstruction. Women with macromastia are the obvious candidates, but women with less volume and considerable ptosis may also be eligible for this procedure. The dermal flap needs to have a certain size to fulfill its purpose, i.e., reaching the border of the pectoralis major muscle while allowing for a sizable implant pocket large enough for sufficient implant projection.
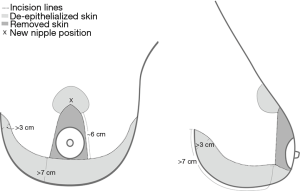
The amount of redundant skin is evaluated by drawing a standard Wise pattern on the patient’s skin. The distance from the inframammary fold (IMF) to the lower part of the Wise pattern (Figure 2), should be no less than 7 cm, and the skin laxity should be such that the medial part of the drawing can arch to give the flap a few cm height at the medial corner.
Previous scars in the IMF may compromise the blood supply of the dermal flap, which should be taken into consideration when planning the procedure.
Preoperative markings
The standard Wise pattern is drawn with the patients in the upright position.
The IMF and the breast meridian and its continuance under the breast are marked. The new position of the nipple is marked on the breast meridian at the level of the IMF or a little higher. Depending on patient build and planned breast size, this point should be between 18 and 23 cm from the sternal notch. A dome-shaped areola (4 cm × 6 cm) is marked. Then, the breast is pushed laterally with moderate tension to draw the medial “leg” of the Wise pattern in alignment with the upper and lower part of the breast meridian. The lateral leg is drawn in a similar fashion. The “legs” of the drawing should be around 6 cm for a medium sized reconstruction. Let the vertical legs meet just below the new nipple position, to avoid a suture line just beneath the nipple graft at the point where the graft is thickest.
The lower part of the Wise pattern is drawn like an S-shape, starting with a large semicircle and towards the medial and lateral end, the line switches direction. This shapes the lower pole to a more rounded, natural appearance, and it gives the dermal flap a little more height medially and laterally (Figure 2).
The vertical legs and the upper edge of the dermal flap form a triangle (Figure 2), and this triangle is the only skin that needs to be removed. Depending on the size and shape of the breast, the nipple may be located within the triangle or below it.
In the very large breast, the breast footprint is often too wide for a standard implant, and the pocket will therefore be too wide and cause lateral displacement or rotation of the implant. A back-cut can be made, to free the dermal flap laterally and attach it to the serratus fascia, in order to reduce the width of the pocket. The length of the back-cut should not exceed the height of the flap. The back-cut should be avoided if there is a previous scar in the IMF.
Surgical technique
Infiltrate the dermal flap intradermally with a diluted solution of lidocaine and adrenaline (max 7 mg/kg diluted to 50 mL per breast) to facilitate de-epithelialization. Take care not to go through the deep part of the dermis, when de-epithelializing the skin, in order to preserve vessels of the subdermal plexus, the main blood supply of the flap.
Cut along the lower line of the Wise pattern, and leave the triangle (Figure 2) on the upper mastectomy flap until the mastectomy is done. This may seem unusual for the oncologic surgeon, in that the tissue under the nipple is removed from the main mastectomy specimen and sent separately. The reason is that if you cut the triangle out primarily and perform the mastectomy, there is a considerable risk of damaging subcutaneous tissue under the corners, which may lead to wound breakdown at the T-junction.
The breast tissue is removed along its superficial fascia, and along the pectoral fascia. Take care not to damage the dense connective tissue sometimes seen along the IMF. Remove the nipple-areola graft from the specimen, and leave it in an isotonic saline solution until needed.
A subpectoral pocket is dissected by lifting up the edge of the pectoralis major muscle and by dividing its costal and sternal attachments up to the level of the nipple graft. Local anaesthetic (Lidocaine with adrenaline 10 mg/mL, max 7 mg/kg) is injected at the sites of the anterior and lateral intercostal nerves, and a pectoral nerve block is injected into the loose connective tissue between the pectoralis minor and major muscles (10).
If the breast is wide, a back-cut can be made along the lower border of the de-epithelialized flap and the abdominal skin, from lateral to medial. This “lateral flap” should not be longer than its width. The lateral flap is sutured to the serratus fascia with interrupted vicryl 3.0 or PDS 3.0 sutures. The dermal flap is sutured to the muscle edge from medial to lateral, with absorbable interrupted 3.0 sutures. Leave a lateral opening to insert the desired implant, and close the pocket. In most cases, you will need to leave a triangle of uncovered implant in the upper lateral corner. Trying to pin down the muscle at this location will cause discomfort for the patient, and should be avoided.
Now, remove the triangle of the Wise pattern (Figure 2), and drape the upper pole skin over the reconstruction. The corners of the inverted T should meet at the breast meridian. A suction drain is placed in the mastectomy pocket. The skin is closed by interrupted 3.0 vicryl sutures and running intradermal monocryl 4.0 sutures.
The nipple-areola graft is trimmed, and all ducts are removed from the center of the nipple. The drawing for the nipple recipient site is adjusted, and the skin is de-epithelialized. The graft is sutured with a running prolene 5.0 suture, and a compressive bolster dressing with Vaseline gauze and surgical sponge is placed, and sutured to the skin by a prolene 3.0 suture.
In cases where a tumor is located close to the nipple (<1 cm), or according to patient preference, a delayed nipple reconstruction can be used instead of a graft.
Post-operative care
Patients wear a non-wired supportive bra for 3 months. If extra support is needed laterally (depending on level of lateral dissection), a foam roll is used for 2 weeks.
The drains are kept in place until the daily accumulation is less than 50 cc, maximum 10 days.
Intravenous antibiotics (cefuroxime 1.5 g) are distributed three times daily until the patient is fully mobilized and well enough to be discharged (usually 1–2 days post-op). The antibiotic treatment is then changed to tablets (dicloxacillin 1 g ×3) until 24 hours after removal of drains. The dressing and sutures around the nipple graft are removed after 5 days.
Patients should refrain from heavy sports during the first six weeks.
Case series
Patient population
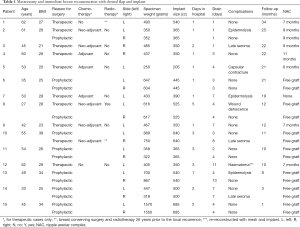
Between March 2016 and January 2019, 15 women aged 27–62 were treated by mastectomy and immediate breast reconstruction with a dermal flap and implant at the Hospital of South West Jutland, Esbjerg, Denmark. Five of these patients were referred for risk reducing surgery after genetic counseling, and treated bilaterally. Ten patients were treated for breast cancer, three bilateral mastectomies, and seven unilateral mastectomies with symmetrizing mastopexy or breast reduction on the contralateral breast (Table 1).
Full table
Results
The 15 women had 23/23 (100%) successful breast reconstructions, 22/23 (96%) of these with a dermal flap (Figure 3). The median hospital stay was 1 day (range, 1–5 days), and the drains were kept for 4 days (range, 1–13 days). The median weight of the breast specimen was 485 g (range, 250–1,570 g), and the median implant size 445 cc (range, 205–685 cc). Four patients had asked for an increase in volume, the rest wanted a volume reduction (Table 1). The median follow-up was 12 months (range, 1–34 months).

There were no cases of implant loss or delayed adjuvant treatment due to complications following surgery. Three patients had a superficial wound at the T-junction that healed without surgical intervention. In all cases with free nipple grafts (14 breasts), there was some epidermolysis of the free nipple graft and loss of projection of the transplanted nipple, but 100% take of the graft (Figure 4). Three patients had acute onset late seroma after strenuous exercise (at 6 weeks, 3 and 13 months, respectively), of which one required puncture, the others were treated conservatively and regressed within a few weeks. One patient had a major complication; 16 days after surgery, she had a sudden haematoma and was reoperated at a different hospital by a surgeon who was not familiar with this procedure. The surgeon opened the cavity by cutting through the IMF incision from medial to lateral, through the base of the flap, and removed the implant. Two days after, she came back to the primary surgeon, who re-reconstructed the patient by removing the now necrotic flap and replaced it with a synthetic mesh (Tigr® Matrix, NovusScientific, Uppsala, Sweden) and a bigger implant. The healing was uneventful.

Comments
The use of a dermal flap for internal support in direct-to-implant breast reconstruction is visualized. The technique can be used for large ptotic breasts and for smaller ptotic breasts with redundant skin. The dermal flap has many advantages compared to the use of acellular dermal matrices or artificial meshes: Acellular dermal matrices may carry the risk of immunological reactions (11) and are quite costly. The patient’s own tissue is more elastic and moldable than the artificial products, and stretches naturally over time, and the double layer of dermis and subcutaneous fat provides good coverage and support of the implant. In cases of wound dehiscence at or around the T-junction, the flap underneath provides extra implant cover and reduces the risk of implant exposure (8). The risk of T-junction breakdown in Wise pattern mastectomies may be as high as 25% (12).
The concept of using de-epithelialized tissue from the lower pole of the breast is not new; internal dermal slings for mastopexy is widely used in massive weight loss patients in various forms (13,14) and for aesthetic augmentation-mastopexy for support of the implant and tissue cover under the T-junction (15). De Vita et al. reported a series of 74 direct to implant breast reconstructions with dermal sling, where they occasionally needed to elevate the serratus muscle to increase the width of the pocket, and also used ADM if the dermal flap could not reach the muscle in the medial aspect (16). The design with a S-shaped incision instead of a straight line, will provide enough flap height in the medial part of the breast in most cases. In addition, the back-cut in the lateral part of the dermal flap has shown to provide good lateral support for the implant without disrupting normal anatomy of the serratus muscle. Nava suggested that the distance from nipple to IMF should be ≥8 cm and sternal notch to nipple ≥25 cm (17). However, we find the nipple position irrelevant in the preoperative evaluation; the new nipple position and the size of the area left under the Wise pattern are the most important anatomical markers.
In some cases, where the skin envelope has been too small for a true dermal flap and implant reconstruction, a balcony-like (15), smaller dermal flap has been used to support the lower pole, as well as using synthetic mesh, but these patients are not reported in this case series.
When planning the procedure, the final breast size is discussed with the patient, since it is possible to adjust implant size and skin excision according to their desires. Most cases with macromastia call for a reduction of volume, and in these cases the implant size can be chosen preoperatively. In many cases, patients ask for the same size or a little larger than current breast volume, and in these cases implant size is chosen during the operation. The thickness of the subcutaneous fat is the same in all areas of the breast, but vary between patients, and range from very thin (1–2 mm) to quite substantial (more than 2 cm). The thicker the fatty layer, the smaller the implant for the same final result. Thicker flaps tend to produce more natural final results. In some patients, the fatty subcutaneous layer may even provide enough volume for a full breast reconstruction (18). Patients with a thinner fatty layer do not seem to have an increased risk of compromised blood supply to the flaps.
We perform the operation using monopolar cautery, and do not inject tumescent solutions before performing the mastectomy. In our experience, tumescent mastectomy tends to blur the planes, and makes the thin fascial layer over the breast difficult to follow—especially in women with fatty breasts and in very skinny patients. Other surgeons advocate tumescence (19), and this is left up to each surgeon, guided by their personal experience.
The dermal flap is a one-stage direct to implant and an inexpensive alternative to the more expensive two-stage Wise pattern mammoplasty and direct-to-implant reconstruction with ADM as described by Gunnarsson et al. (7). If performed properly, this technique is easy and safe, and the subdermal network provides sufficient vascular supply. However, if there are previous scars in the IMF, the flow through the subdermal plexus may not be enough to nourish the flap. This should be taken into consideration when planning the flap. A short IMF scar in a wide breast should not pose a problem since collateral vessels will supply the flap from the areas medial and lateral of the scar. It would be unwise to do a back-cut in these cases, since it will cut off the lateral blood supply.
This technique requires that you trust your colleagues; if the de-epithelialization is too deep or if the mastectomy plane has been too superficial, the blood supply of the flap may be damaged, which may lead to necrosis of the flap.
Conclusions
Immediate breast reconstruction using a dermal flap and an implant is a safe, quick one-stage procedure.
Acknowledgments
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Freeman BS. Subcutaneous mastectomy for benign breast lesions with immediate or delayed prosthetic replacement. Plast Reconstr Surg 1962;30:676-82. [Crossref] [PubMed]
- Salzberg CA, Ashikari AY, Berry C, et al. Acellular dermal matrix-assisted direct-to-implant breast reconstruction and capsular contracture: A 13-year experience. Plast Reconstr Surg 2016;138:329-37. [Crossref] [PubMed]
- Salzberg CA. Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg 2006;57:1-5. [Crossref] [PubMed]
- Gunnarsson GL, Thomsen JB. Prepectoral Hammock and Direct-to-implant Breast Reconstruction in 10 Minutes: A Focus on Technique. Plast Reconstr Surg Glob Open 2018;6:e1931. [Crossref] [PubMed]
- Jacobs JM, Salzberg CA. Implant-based breast reconstruction with meshes and matrices: biological vs synthetic. Br J Hosp Med (Lond) 2015;76:211-6. [Crossref] [PubMed]
- Bostwick J. Implant reconstruction with breast skin and volume reduction using an inverted T-incision. In: Bostwick J. editor. Plastic and reconstructive breast surgery. 2nd ed. St Louis: Quality Medical Publishing, 1990:1369-73.
- Gunnarsson GL, Bille C, Reitsma LC, et al. Prophylactic Nipple-Sparing Mastectomy and Direct-to-Implant Reconstruction of the Large and Ptotic Breast: Is Preshaping of the Challenging Breast a Key to Success? Plast Reconstr Surg 2017;140:449-54. [Crossref] [PubMed]
- Hansson E, Jepsen C, Hallberg H. Breast reconstruction with a dermal sling: a systematic reviewof surgical modifications. J Plast Surg Hand Surg 2019;53:1-13. [Crossref] [PubMed]
- Carstensen L. Immediate breast reconstruction with dermal flap and implant. Pre-operative markings, surgical procedure and final results are shown in this video. Asvide 2019;6:290. Available online: http://www.asvide.com/watch/32975
- Blanco R. The “pecs block”: a novel technique for providing analgesia after breast surgery. Anaesthesia 2011;66:847-8. [Crossref] [PubMed]
- Ganske I, Hoyler M, Fox SE, et al. Delayed hypersensitivity reaction to acellular dermal matrix in breast reconstruction: the red breast syndrome? Ann Plast Surg 2014;73:S139-43. [Crossref] [PubMed]
- Kilgo MS, Kaufman GJ, Shen AE, et al. A comparison of elliptical mastectomy to inverted-T pattern mastectomy in two-stage prosthetic breast reconstruction. Plast Reconstr Surg 2015;136:e426-33. [Crossref] [PubMed]
- Rubin J. Mastopexy after massive weight loss: dermal suspension and total parenchymal reshaping. Aesthet Surg J 2006;26:214-22. [Crossref] [PubMed]
- Colwell AS, Breuing KH. Improving shape and symmetry in mastopexy with autologous or cadaveric dermal slings. Ann Plast Surg 2008;61:138-42. [Crossref] [PubMed]
- Vita R, De , Zoccali G, Buccheri EM. The Balcony Technique of Breast Augmentation and Inverted-T Mastopexy With an Inferior Dermoglandular Flap. Aesthet Surg J 2017;37:1114-23. [Crossref] [PubMed]
- De Vita R, Pozzi M, Zoccali G, et al. Skin-reducing mastectomy and immediate breast reconstruction in patients with macromastia. J Exp Clin Cancer Res 2015;34:120. [Crossref] [PubMed]
- Nava MB, Cortinovis U, Ottolenghi J, et al. Skin-reducing mastectomy. Plast Reconstr Surg 2006;118:603-10. [Crossref] [PubMed]
- Richardson H, Ma G. The Goldilocks mastectomy. Int J Surg 2012;10:522-6. [Crossref] [PubMed]
- Shoher A, Hekier R, Lucci A. Mastectomy performed with scissors following tumescent solution injection. J Surg Oncol 2003;83:191-3. [Crossref] [PubMed]