Optimal assessment tools in assessing breast surgery: patient reported outcome measures (PROMs) vs. objective measures
Introduction
Improving the health-related quality of life (HRQoL) of patients is a fundamental aim of medicine. This applies in the field of breast surgery. The success of aesthetic breast surgery is measured by the extent to which patients’ physical, psychological and social well-being are enhanced. Breast cancer-related surgery is increasingly focusing on these outcomes. In Australia, breast cancer mortality continues to fall while incidence rises (1). With one in eight females diagnosed with breast cancer before the age of 85 and 5-year survival rates over 90%, the focus of research has shifted towards improving survivors’ quality of life (QoL).
Selecting optimal assessment tools for assessing breast surgery outcomes is vital to obtaining meaningful results. Patient reported outcome measures (PROMs) are now recognised as valuable tools for collecting outcomes data in areas previously overlooked by traditional objective measures. Assessing breast surgery HRQoL outcomes, such as satisfaction, functionality and well-being, from the patient perspective provides essential information required to improve the shared decision-making process. With increasing use of PROMs, it is important to consider their place in relation to conventional objective measures to optimise future breast surgery research.
Methods
This study was conducted as a narrative review. The authors undertook a literature search of Ovid MEDLINE using the MeSH terms: patient reported outcome measures, quality of life, functional outcomes, aesthetic outcomes, complications, and breast surgery. Only published articles in English language were included. No articles were excluded on the basis of year of publication; the oldest relevant article identified was published in 1990. Reference lists were also examined to find relevant articles not detected through the search. All articles relevant to the use of PROMs in breast cancer or aesthetic surgery were included in preparing the review.
PROMs
Along with the expectation for clinicians to provide holistic, patient-centred care, there has been growing acceptance of the value of assessing outcomes from the patients’ perspective. PROMs allow patients to quantify their symptoms, function, and QoL in relation to a disease, treatment, or both (2,3). In breast surgery, PROMs ultimately enable patients to evaluate the impact and effectiveness of the intervention. This is in contrast to objective measures which are calculated in an unbiased fashion without consideration for the patient experience. While objective measures have an essential role in identifying specific risks and benefits of surgery, they fail to adequately assess many outcomes of tremendous importance to patients. Well-being (physical, psychological and social) and overall QoL are critical outcomes of breast surgery which are best judged by the patient.
PROMs have the potential to improve to health outcomes by providing evidence-based information to patients, thereby supporting them to make informed decisions regarding their management (2). This is especially relevant in breast surgery where QoL outcomes weigh heavily on treatment decisions. Aesthetic outcomes, functionality and well-being are often key considerations of women choosing between surgical options, and thus robust research in these areas is imperative for informed decision making. The importance of optimising the decision-making process was highlighted in a recent systematic review, which revealed that decisional regret following mastectomy was associated with insufficient and unclear information provided prior to surgery (4). In addition, patient support for future use of PROMs was highlighted in a study by Lagendijk et al., in which 89% of breast cancer participants agreed that PROMs had the potential to improve quality of care, and over 80% believed that PROMs could have been used as a ‘guidance tool for themselves’ during their treatment journey (5).
PROMs can be broadly broken down into two categories; generic and specific. Specific instruments have been developed to assess an individual symptom, disease or intervention, while generic instruments have not (6). Generic tools have the benefit of measuring general QoL outcomes in a large range of conditions, however, they are often not sensitive enough to detect changes due to specific interventions. For example, a generic questionnaire may be able to detect differences in overall physical function following breast surgery but not a change in breast symmetry. Disease and intervention specific instruments are more responsive to surgical change and are usually considered superior for assessing breast surgery outcomes (7,8). Furthermore, PROM instruments must be developed and validated in a method to ensure they demonstrate reliability, validity and responsiveness for their results to have meaning (6,8,9). An instrument is considered to be reliable if the results are reproducible and consistent, valid if it is capable of measuring what it intends to measure, and responsive if it is sensitive enough to detect change. While hundreds of PROM instruments have been used to assess breast surgery outcomes, there have been few developed and validated to achieve these criteria (8).
Frequently used PROMs
While individual surgeons and hospitals have begun to adopt PROMs in both research and clinical settings, widespread use has been limited (2). Large-scale applications of PROMs such as the first national voluntary audit of mastectomy and breast reconstruction in England in 2008 (10) and mandatory audits of all providers of hip and knee replacement, groin hernia repair and varicose vein surgery (2) have shown that PROMs can be successfully implemented in large cohorts. The BREAST-Q™ and The European Organisation of Research and Treatment of Cancer’s Quality of Life Questionnaire (EORTC QLQ) are two validated PROMs which have been widely utilised in breast surgery outcome assessment.
BREAST-Q™
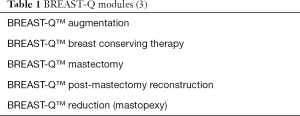
Breast-Q™ is a validated PROM which has been extensively used by both researchers and clinicians to assess the impact and effectiveness of breast surgery (9,11). The instrument was developed in 2009 in accordance with international PROM guidelines and criteria, and has since been translated into 30 languages (3). BREAST-Q™ is available for non-profit academic research and for use in clinical care free of charge. Since its inception, BREAST-Q™ has developed five modules, as listed in Table 1. All modules consist of three QoL domains (psychosocial well-being, physical well-being and sexual well-being) and three satisfaction domains (satisfaction with breasts, satisfaction with outcome and satisfaction with care) (9). A recent systematic review by Liu et al. identified 54 peer-review articles which had used BREAST-Q™ to assess patient reported outcomes following oncoplastic breast surgery, including four Australian studies (9). To date, studies utilising BREAST-Q™ have increased our understanding of breast surgery related outcomes, particularly in relation to patient education, timing of reconstruction, implant type and fat grafting (3,9).
EORTC QLQ
The EORTC QLQ-C30 is the most widely used questionnaire in Europe for assessing patient reported outcomes, and has been adopted globally (12). The questionnaire consists of 30 core items and aims to address general concerns and symptoms of cancer patients, such as fatigue and pain (13). It is not, however, sensitive enough to capture issues unique to specific malignancies and should be used alongside supplementary modules. The EORTC-QLQ-BR23 is a breast cancer specific module that was developed to complement the generic questionnaire. It has been internationally scrutinised, and is considered to be a valid and reliable tool for assessing breast cancer related QoL (13). Unlike the BREAST-Q™, the EORTC modules are only intended for use in malignancy and have no role in evaluating breast surgeries such as breast augmentation or reduction.
Limitations of PROMs
Assessing outcomes from patients’ perspectives will fill a significant gap in breast surgery research, however, there are limitations of PROMs which should be considered. The nature of requesting patients, some of who may not recognise the benefit of their participation, to complete questionnaires can result in poor response rates. There has been significant variation in response rates in studies that have used PROMs in breast surgery. A recent review by Liu et al. showed that studies using BREAST-Q™ stated reported response rates from 32% to 100% (9). Additionally, poor response rates are compounded by response bias. Those who are deeply satisfied or dissatisfied will often be overrepresented, as is the case in surveys and feedback questionnaires not limited to medicine (3). A study by Hutchings et al. found that patients from more deprived backgrounds, who were younger, sicker and non-White were underrepresented in the national audit of various elective surgeries in England (14). This must be kept in mind when considering whether findings are applicable to individual patients seeking advice in a clinical setting. The use of information technology, such as electronic, emailed and app versions of questionnaires, will likely increase response rates and potentially allow patients to give more accurate answers to sensitive questions in the comfort of their own home.
PROMs vs. objective measures
Selecting the optimal assessment tool is an essential aspect of any study design and will influence the significance of the results. With increasing evidence demonstrating that PROMs have utility in evaluating breast surgery outcomes, it is important to consider their role in relation to objective measures. Some outcomes can only be measured with precision objectively, and thus objective measures will always have value in surgical research. However, there are also outcomes traditionally assessed through objective measures which may be more appropriately assessed from the patient’s perspective. It is important to recognise these instances in order to increase understanding of breast surgery outcomes, advance surgical care and improve patients’ QoL.
Survival
Survival and mortality are of immense importance in breast surgery considering the small but significant risk of death associated with any operation, as well as mortality related to malignancy in breast cancer surgery. These critical outcomes can be clearly and accurately assessed using objective measures, and are not suitable for assessment through PROMs. Noteworthy studies have demonstrated that radical mastectomy and breast-conserving therapy (BCT) followed by post-operative radiotherapy result in equivalent survival in women with early breast cancer (15,16). Fisher et al. observed no significant differences with respect to disease-free survival, distant disease survival and overall survival (15), while Veronesi and colleagues also found identical long-term survival rates in these groups (16). Insights from these studies have influenced the surgical decisions of hundreds of thousands of women worldwide each year (16). Objectively measuring mortality and survival will remain an essential focus of future research comparing surgical approaches, especially in breast cancer surgery.
Survival and mortality are not only relevant for patients choosing between surgical options, but also for patients considering prophylactic mastectomy. Patients with high genetic risk for developing breast cancer, such as those with a BRCA mutation, require accurate data regarding their risk of malignancy and mortality, as well as the expected benefit of preventative mastectomy, to make informed decisions regarding treatment. In a recent study, Kuchenbaecker and colleagues identified that the cumulative breast cancer risk to age 80 years was 72% and 69% for patients carrying BRCA1 and BRCA2 mutations, respectively (17). In addition, Giannakeas and Narod examined the mortality benefit of mastectomy in a BRCA cohort through a simulated analysis, highlighting that the mortality benefit of early mastectomy declines with delay of surgery (18). These studies have provided crucial evidence for women considering prophylactic mastectomy through assessing objective outcomes surrounding incidence and mortality. While PROMs may have value assessing patients’ psychological well-being, for example cancer worry or peace of mind, decreasing mortality risk will remain the key focus of prophylactic mastectomy and thus objective measurement in this area is paramount.
Complications
Identifying complications and risk factors associated with their occurrence is important for selection criteria and perioperative planning to improve outcomes in breast surgery (19). Patients can provide valuable insights regarding their experience of complications as well as their impact on future QoL. Objective measures on the other hand, may provide more accurate details regarding complication rates and their severity. While optimising patient outcomes is the central aim, there are other significant consequences of surgery separate to the patient experience that should also be considered, such as utilisation of resources and costs associated with complications. It is likely that applying a combination of objective measures and PROMs is necessary to accurately capture the full spectrum of complications and their impact in breast surgery.
Short-term complications
Post-operative complications cause significant morbidity, and even mortality, and are rightly a major focus of surgical research. Short-term complications can be further subdivided into major and minor events, with major events often described as complications which require additional surgical intervention, readmission into hospital, or prolonged hospital admission for further treatment (20,21). Examples of short-term complications include infection, wound dehiscence, haematoma, seroma, implant failure, tissue necrosis, pulmonary embolism, and post-operative pain. With the exception of post-operative pain, these events are most frequently measured objectively in terms of their rate of occurrence. Furthermore, measures assessing the severity of these complications are almost universally objective, for example drain outputs, units of blood transfused and length of hospital admission. It would be inappropriate for patients to evaluate complications for the purpose of comparing interventions, since this information can be more accurately obtained clinically. PROMs, however, may have value when assessing the effect of complications. Evidence-based data regarding QoL following complications would enable clinicians to not only explain the risks of procedure, but the likely impact if they were to occur.
Post-operative pain, unlike other short-term complications, cannot be measured objectively since pain is itself subjective. The visual analogue scale (VAS) has been widely used to assess pain from the patient’s perspective in numerous clinical situations, including post-operatively in breast surgery (22,23). Multiple studies have attempted to assess post-operative pain objectively through measuring patients’ analgesic requirement, however, this may be influenced by factors other than the patient’s pain, for example their willingness to take medications and staff attitudes (22,23).
Long-term complications
With improvements in life expectancy following breast cancer treatment, assessing the prevalence and impact of long-term complications is increasingly relevant (24). Lymphedema is a common complication in breast cancer patients in which there is chronic accumulation of lymphatic fluid in the upper limb following disturbance or infiltration of lymphatic channels (25,26). This can be either due to tumour invasion or a result of treatment, with both breast surgery and radiotherapy frequently implicated (24). There are many morbidities associated with upper limb lymphedema, including but not limited to infection, pain, decreased range of movement and function, and skin changes, which ultimately result in decreased functionality and QoL (25). While lymphedema is often clinically defined using objective measures, such as arm circumference and volume (25), omitting patient reported symptoms risks failing to capture the true prevalence and effect of this complication. As the impacts of lymphedema mainly surround function and QoL, PROMs may be more suitable in assessment. There have been numerous PROMs developed which include evaluation for lymphedema, as well as instruments developed specifically for breast cancer related lymphedema (27,28). A study by Ahmed et al. identified that both women with diagnosed lymphedema and women with arm symptoms without a diagnosis of lymphedema had lower HRQoL compared to breast cancer survivors without a diagnosis or arm symptoms (25). Furthermore, only 2% of women with arm symptoms without a diagnosis of lymphedema had received some form of treatment compared with 52% of patients with a diagnosis, highlighting that incorporating PROMs into post-surgical review may improve treatment rates.
Aesthetic outcomes
Aesthetic results, and their ramifications, are often personal and sensitive concerns following breast surgery. Whether the primary aim of the procedure is to optimise a patient’s satisfaction with their breasts, as is often the case in breast augmentation, reduction and reconstruction, or minimising deformation as a secondary aim in the case of breast cancer surgery, cosmetic outcome is nearly always of interest to the patient. Not surprisingly, studies have demonstrated that aesthetic outcome is closely related to QoL following breast cancer surgery (29,30). While the importance of aesthetic outcome is well recognised, there remains no gold standard tool of assessment (31). Methods for evaluating aesthetic outcomes following breast surgery can be broadly categorised as either subjective or objective, both which have inherent limitations.
Aesthetic outcome can be subjectively evaluated by the patient or an observer (32). Assessing aesthetic outcome using PROMs appears the most instinctively appropriate method as only the patient can reveal whether they are satisfied with the result (33), however, there are many factors which influence this outcome irrelevant to the clinical situation and intervention (33). Patient age, socioeconomic status, expectations and psychological adaptations, as well as many other factors likely to be unknown to investigators, have the ability to impact a patient’s perspective on aesthetic result, and are difficult to control for (34,35).
Assessment from an observer removes the influence of many confounding factors at the expense of overlooking the patient’s perspective. A number of tools have been developed to help clinicians evaluate aesthetic outcome, including the widely used Harris Scale, which can either be applied during a consultation with the patient or by analysing photographs (31). However, a number of issues regarding the use of subjective measures have been recognised (31,34). Thoroughly assessing cosmetic result using these tools can be time-consuming for specialists, and studies have demonstrated poor inter-observer agreement, which is intrinsic to the subjective nature of the assessment (31).
Alternatively, objective measures can be utilised to assess aesthetic outcomes. Current objective methods measure asymmetries between the treated and non-treated breast, either by directly assessing the patient or photographs (32). The perceived benefits of an objective assessment tool include increased reproducibility and non-biased results, allowing for more accurate outcome based research (32). Furthermore, computerised evaluation tools could potentially allow for simple, instantaneous assessment without the need for a trained observer, such as a breast or plastic surgeon (32). Two software programs have been developed in recent years to achieve these goals in BCT. The Breast Cancer Conservative Treatment cosmetic results (BCCT.core) is a semi-automatic program which analyses 2-dimensional torso photographs, assessing a number of elements related to asymmetry, volume, colour differences, and scar appearance, whereas the Breast Analysing Tool (BAT) only measures differences in asymmetry (32,33). Studies have demonstrated that the BCCT.core has good concordance between users, however, poor concordance with PROMs and subjective assessment by specialists (32,33). This may be because tool can only focus on measureable asymmetries and is unable to capture the global aesthetic outcome which is arguably more important (32).
Due to inbuilt limitations of both subjective and objective measures, it is likely both approaches need to be applied to comprehensively assess aesthetic outcomes in breast surgery (33).
HRQoL outcomes
The value of assessing HRQoL outcomes has now been recognised in all fields of breast surgery. The goal of non-cancer related breast surgery has long revolved around improving QoL, whereas falling mortality following breast cancer related surgery has resulted in increased focus on survivorship QoL. It is generally accepted that there are three key domains of HRQoL; physical, psychological and social (6,7). Physical refers to bodily functioning or dysfunction as it is perceived by the patient. Psychological encompasses areas related to the mind, including mood and thoughts. Finally, social relates to carrying out activities as part of society (6). All three aspects of HRQoL can be impacted, positively or negatively, by breast surgery. Robust, evidence-based data regarding HRQoL outcomes is vital for patients when considering surgical options.
Physical well-being
Upper limb dysfunction is unfortunately not a rare outcome following breast surgery, and is characterised by weakness, decreased range of movement, pain, lymphedema, and ultimately decreased function (36). Significant research has been undertaken to find an effective treatment for upper limb dysfunction considering the debilitating effect it has on many women following breast cancer surgery (36-38). Studies have used a combination of PROMs and objective measures when evaluating upper limb dysfunction. Shoulder range of movement, muscular strength and even surface electromyography have been utilised to objectively assess arm functionality (36,37,39). These can provide clear, unbiased data following breast surgery but may not be an accurate representation of the real-life implications of upper limb dysfunction. Alternatively, PROMs can be used to gauge the impact upper limb symptoms are having on the patient and their day to day function. The PROSPER trial (Prevention of Shoulder Problems Trial), currently underway in the UK, is using the Disabilities or the Arm, Shoulder, and Hand (DASH) questionnaire, to assess the effectiveness of an early supervised exercise program in preventing shoulder problems (38). The DASH questionnaire is a specific 30-item PROM constructed to identify difficulties with daily tasks as a result of upper limb pathology. While the DASH and other PROM questionnaires may give superior insight into arm functionality, they have the potential to be influenced by confounding factors. For these reasons, there is no universally accepted measure of upper limb dysfunction, and it is likely a combination of objective and subjective measures is necessary for accurate, comprehensive results.
Many patients who undergo breast surgery are part of the workforce, and hence, assessing changes in working performance can provide valuable insight into the impact surgery has had on their function. Symptoms and physical limitations can lead to decreased productivity, workplace and role modifications, delay in returning to work, and even unemployment (40). Workplace performance can be evaluated subjectively using PROMs or objectively, through measuring items such as time to return to work or decrease in hours worked per week. A recent systematic review by Zomkowski et al. identified 13 studies which assessed physical symptoms and working performance in female breast cancer survivors utilising either interviews, questionnaires, objective measures, or a combination of these (40), highlighting there is no universally accepted assessment tool.
Psychological and social well-being
Breast surgery can drastically impact upon patients’ psychosocial well-being given that breasts are frequently associated with femininity and sexuality. Changes in confidence, self-esteem and body image as a result of breast surgery can result in decreased feelings of sexual attractiveness, satisfaction in sex life and sexual activity (8). These outcomes are irrefutably personal in nature and impossible to measure without patients’ subjective input. Multiple PROMs have been developed to assess psychosocial well-being following breast surgery, including the validated BREAST-Q™ which purposely includes psychosocial well-being and sexual well-being domains (9,41).
Rigorous research in this area is essential for surgical decision making as PROMs have already demonstrated that different surgical approaches are associated with varying psychosocial outcomes (42-45). Mastectomy and BCT have been frequently compared. BCT has consistently demonstrated to have significantly less negative influence on body image and feelings of being sexually desirable than mastectomy (42-45), with Rowland et al. ultimately identifying that BCT had less negative impact on women’s sex lives than mastectomy, with or without reconstruction (42). The value women place on this was highlighted in Noguchi et al.’s paper where 83% of patients who underwent BCT stated they would select this as their future treatment of choice, whereas 62% of patient who had mastectomy with immediate breast reconstruction would not elect for the same treatment again (45). Surprisingly, studies have shown that there is no difference in fear of breast cancer recurrence following mastectomy or BCT, with both groups unfortunately having high rates of continued concern (42,45).
The benefit of post mastectomy breast reconstruction has also been a focus of significant research. A number of studies utilising BREAST-Q™ have shown superior psychosocial and sexual well-being in women who elect for reconstruction compared to women who have mastectomy alone (46-48). There are, however, additional aspects for patients and clinicians to consider, including type and timing of reconstruction, choices which may affect QoL. For instance, autologous reconstruction using transverse rectus abdominis musculocutaneous (TRAM) flaps have shown to be associated with superior body image when compared to prosthetic implants (3,49). In terms of timing, studies have discovered that the vast majority of patients who undergo immediate breast reconstruction following mastectomy maintain a post-procedure preference for this option while those who have delayed reconstruction would have in hindsight preferred immediate reconstruction (50,51), however, a systematic review by Winters et al. found there was a lack of high quality studies assessing PROMs in this area (7). Further research using validated PROMs will likely allow patients to make more educated, evidenced based decisions in breast reconstruction.
Conclusions
Selecting optimal assessment tools for evaluating breast surgery is an essential step to obtaining meaningful outcome data. Clear, accurate HRQoL outcomes data is essential for patients to make informed treatment decisions which reflect their values. The introduction of PROMs has improved assessment of QoL outcomes, with tools such as BREAST-Q™ and EORTC QLQ contributing significantly to our understanding of breast surgery results. Future utilisation of PROMs will not only provide vital information for shared decision making, but has the potential to aid the development of decision aids and patient education programs as well as influencing healthcare policy and resource allocation.
While the outlook for PROMs is promising, objective measures still have a clear role in breast surgery research and should continue to be utilised where appropriate. It appears that PROMs are the most suitable assessment tool for assessing physical, psychological and social well-being following breast surgery, as only patients can provide insight into these outcomes. PROMs may also offer valuable perceptions into the impact of complications and aesthetic outcomes alongside objective measures. On the contrary, mortality and complication rates remain most appropriately assessed by objective measures.
In summary, it is evident that there is no one optimal assessment tool for assessing breast surgery outcomes. A combination of PROMs and objective measures is necessary to accurately and comprehensively evaluate the impact and effectiveness of surgical breast interventions.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Australian Institute of Health and Welfare. Cancer in Australia 2017. Canberra: AIHW, 2017.
- Black N. Patient reported outcome measures could help transform healthcare. BMJ 2013;346:f167. [Crossref] [PubMed]
- Cohen WA, Mundy LR, Ballard TNS, et al. The BREAST-Q in surgical research: A review of the literature 2009–2015. J Plast Reconstr Aesthet Surg 2016;69:149-62. [Crossref] [PubMed]
- Flitcroft K, Brennan M, Spillane A. Decisional regret and choice of breast reconstruction following mastectomy for breast cancer: A systematic review. Psychooncology 2018;27:1110-20. [Crossref] [PubMed]
- Lagendijk M, van Egdom LSE, Richel C, et al. Patient reported outcome measures in breast cancer patients. Eur J Surg Oncol 2018;44:963-8. [Crossref] [PubMed]
- Langenhoff BS, Krabbe PFM, Wobbes T, et al. Quality of life as an outcome measure in surgical oncology. Br J Surg 2001;88:643-52. [Crossref] [PubMed]
- Winters ZE, Benson JR, Pusic AL. A systematic review of the clinical evidence to guide treatment recommendations in breast reconstruction based on patient- reported outcome measures and health-related quality of life. Ann Surg 2010;252:929-42. [Crossref] [PubMed]
- Pusic AL, Chen CM, Cano S, et al. Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patient-reported outcomes instruments. Plast Reconstr Surg 2007;120:823-37; discussion 838-9. [Crossref] [PubMed]
- Liu LQ, Branford OA, Mehigan S. BREAST-Q Measurement of the Patient Perspective in Oncoplastic Breast Surgery: A Systematic Review. Plast Reconstr Surg Glob Open 2018;6:e1904. [Crossref] [PubMed]
- Jeevan R, Cromwell DA, Browne JP, et al. Findings of a national comparative audit of mastectomy and breast reconstruction surgery in England. J Plast Reconstr Aesthet Surg 2014;67:1333-44. [Crossref] [PubMed]
- Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 2009;124:345-53. [Crossref] [PubMed]
- Fayers P, Bottomley A. Quality of life research within the EORTC—the EORTC QLQ-C30. Eur J Cancer 2002;38:S125-33. [Crossref] [PubMed]
- Nguyen J, Popovic M, Chow E, et al. EORTC QLQ-BR23 and FACT-B for the assessment of quality of life in patients with breast cancer: a literature review. J Comp Eff Res 2015;4:157. [Crossref] [PubMed]
- Hutchings A, Neuburger J, Grosse Frie K, et al. Factors associated with non-response in routine use of patient reported outcome measures after elective surgery in England. Health Qual Life Outcomes 2012;10:34. [Crossref] [PubMed]
- Fisher B, Anderson S, Bryant J, et al. Twenty-Year Follow-up of a Randomized Trial Comparing Total Mastectomy, Lumpectomy, and Lumpectomy plus Irradiation for the Treatment of Invasive Breast Cancer. N Engl J Med 2002;347:1233-41. [Crossref] [PubMed]
- Veronesi U, Cascinelli N, Mariani L, et al. Twenty-Year Follow-up of a Randomized Study Comparing Breast-Conserving Surgery with Radical Mastectomy for Early Breast Cancer. N Engl J Med 2002;347:1227-32. [Crossref] [PubMed]
- Kuchenbaecker KB, Hopper JL, Barnes DR, et al. Risks of breast, ovarian, and contralateral breast cancer for brca1 and brca2 mutation carriers. JAMA 2017;317:2402-16. [Crossref] [PubMed]
- Giannakeas V, Narod SA. The expected benefit of preventive mastectomy on breast cancer incidence and mortality in BRCA mutation carriers, by age at mastectomy. Breast Cancer Res Treat 2018;167:263-7. [Crossref] [PubMed]
- Davies K, Allan L, Roblin P, et al. Factors affecting post-operative complications following skin sparing mastectomy with immediate breast reconstruction. Breast 2011;20:21-5. [Crossref] [PubMed]
- Lin KY, Blechman AB, Brenin DR. Implant-based, two-stage breast reconstruction in the setting of radiation injury: an outcome study. Plast Reconstr Surg 2012;129:817-23. [Crossref] [PubMed]
- Romics L, Macaskill EJ, Fernandez T, et al. A population-based audit of surgical practice and outcomes of oncoplastic breast conservations in Scotland–An analysis of 589 patients. Eur J Surg Oncol 2018;44:939-44. [Crossref] [PubMed]
- Byager N, Hansen M, Mathiesen O, et al. The analgesic effect of wound infiltration with local anaesthetics after breast surgery: a qualitative systematic review. Acta Anaesthesiol Scand 2014;58:402-10. [Crossref] [PubMed]
- Campbell I, Cavanagh S, Creighton J, et al. To infiltrate or not? Acute effects of local anaesthetic in breast surgery. ANZ J Surg 2015;85:353-7. [Crossref] [PubMed]
- Erickson VS, Pearson ML, Ganz PA, et al. Arm Edema in Breast Cancer Patients. J Natl Cancer Inst 2001;93:96-111. [Crossref] [PubMed]
- Ahmed RL, Prizment A, Lazovich D, et al. Lymphedema and Quality of Life in Breast Cancer Survivors: The Iowa Women's Health Study. J Clin Oncol 2008;26:5689-96. [Crossref] [PubMed]
- Rockson SG. Lymphedema. Am J Med 2001;110:288-95. [Crossref] [PubMed]
- Mirolo BR, Bunce IH, Chapman M, et al. Psychosocial benefits of postmastectomy lymphedema therapy. Cancer Nurs. 1995;18:197-205. [Crossref] [PubMed]
- Launois R, Megnigbeto A, Pocquet K, et al. A specific quality of life scale in upper limb lymphedema: the ULL-27 questionnaire. Lymphology 2002;35:181-7.
- Heil J, Czink E, Golatta M, et al. Change of aesthetic and functional outcome over time and their relationship to quality of life after breast conserving therapy. Eur J Surg Oncol 2011;37:116-21. [Crossref] [PubMed]
- Heil J, Holl S, Golatta M, et al. Aesthetic and functional results after breast conserving surgery as correlates of quality of life measured by a German version of the Breast Cancer Treatment Outcome Scale (BCTOS). Breast 2010;19:470-4. [Crossref] [PubMed]
- Preuss J, Lester L, Saunders C. BCCT.core – Can a computer program be used for the assessment of aesthetic outcome after breast reconstructive surgery? Breast 2012;21:597-600. [Crossref] [PubMed]
- Cardoso MJ, Cardoso JS, Wild T, et al. Comparing two objective methods for the aesthetic evaluation of breast cancer conservative treatment. Breast Cancer Res Treat 2009;116:149-52. [Crossref] [PubMed]
- Heil J, Dahlkamp J, Golatta M, et al. Aesthetics in Breast Conserving Therapy: Do Objectively Measured Results Match Patients’ Evaluations? Ann Surg Oncol 2011;18:134-8. [Crossref] [PubMed]
- Santos G, Urban C, Edelweiss MI, et al. Long-Term Comparison of Aesthetical Outcomes After Oncoplastic Surgery and Lumpectomy in Breast Cancer Patients. Ann Surg Oncol 2015;22:2500-8. [Crossref] [PubMed]
- Matthews H, Carroll N, Renshaw D, et al. Predictors of satisfaction and quality of life following post-mastectomy breast reconstruction. Psychooncology 2017;26:1860-5. [Crossref] [PubMed]
- McNeely ML, Campbell K, Ospina M, et al. Exercise interventions for upper‐limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev 2010.CD005211. [PubMed]
- Eyjolfsdottir H, Haraldsdottir B, Ragnarsdottir M, et al. A Prospective Analysis on Functional Outcomes Following Extended Latissimus Dorsi Flap Breast Reconstruction. Scand J Surg 2017;106:152-7. [Crossref] [PubMed]
- Bruce J, Williamson E, Lait C, et al. Randomised controlled trial of exercise to prevent shoulder problems in women undergoing breast cancer treatment: study protocol for the prevention of shoulder problems trial (UK PROSPER). BMJ Open 2018;8:e019078. [Crossref] [PubMed]
- Yang EJ, Kwon Y. Changes in shoulder muscle activity pattern on surface electromyography after breast cancer surgery. J Surg Oncol 2018;117:116-23. [Crossref] [PubMed]
- Zomkowski K, Cruz de Souza B, Pinheiro da Silva F, et al. Physical symptoms and working performance in female breast cancer survivors: a systematic review. Disabil Rehabil 2018;40:1485-93. [Crossref] [PubMed]
- Chen CM, Cano SJ, Klassen AF, et al. Measuring Quality of Life in Oncologic Breast Surgery: A Systematic Review of Patient-Reported Outcome Measures. Breast J 2010;16:587-97. [Crossref] [PubMed]
- Rowland JH, Desmond KA, Meyerowitz BE, et al. Role of Breast Reconstructive Surgery in Physical and Emotional Outcomes Among Breast Cancer Survivors. J Natl Cancer Inst 2000;92:1422-9. [Crossref] [PubMed]
- Schain WS, d'Angelo TM, Dunn ME, et al. Mastectomy versus conservative surgery and radiation therapy. Psychosocial consequences. Cancer 1994;73:1221-8. [Crossref] [PubMed]
- Margolis G, Goodman RL, Rubin A. Psychological Effects of Breast-Conserving Cancer Treatment and Mastectomy. Psychosomatics 1990;31:33-9. [Crossref] [PubMed]
- Noguchi M, Kitagawa H, Kinoshita K, et al. Psychologic and cosmetic self‐assessments of breast conserving therapy compared with mastectomy and immediate breast reconstruction. J Surg Oncol 1993;54:260-6. [Crossref] [PubMed]
- Dean NR, Yip JM, Birrell S. Rotation flap approach mastectomy. ANZ J Surg 2013;83:139-45. [Crossref] [PubMed]
- Eltahir Y, Werners LL, Dreise MM, et al. Quality-of-Life Outcomes between Mastectomy Alone and Breast Reconstruction: Comparison of Patient-Reported BREAST-Q and Other Health-Related Quality-of-Life Measures. Plast Reconstr Surg 2013;132:201e-209e. [Crossref] [PubMed]
- Ng SK, Hare RM, Kuang RJ, et al. Breast Reconstruction Post Mastectomy: Patient Satisfaction and Decision Making. Ann Plast Surg 2016;76:640-4. [Crossref] [PubMed]
- Atisha D, Alderman AK, Lowery JC, et al. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg 2008;247:1019-28. [Crossref] [PubMed]
- Al-Ghazal SK, Sully L, Fallowfield L, et al. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol 2000;26:17-9. [Crossref] [PubMed]
- Fernández-Delgado J, López-Pedraza MJ, Blasco JA, et al. Satisfaction with and psychological impact of immediate and deferred breast reconstruction. Ann Oncol 2008;19:1430-4. [Crossref] [PubMed]