Acute non-traumatic adrenal haemorrhage—management, pathology and clinical outcomes
Introduction
Adrenal haemorrhage is an uncommon condition, with reported incidence of 0.14–1.1% on post-mortem studies (1,2). It is difficult to recognize clinically as the presentations are non-specific and vary in severity, particularly in patients with other concurrent illnesses. Failure in early diagnosis of bilateral adrenal haemorrhage may lead to death as a result of untreated primary adrenal insufficiency (3,4). Primary adrenal insufficiency becomes clinically profound only after 90% of the adrenal cortex is compromised (4).
Non-traumatic adrenal haemorrhage has been reported in association with underlying stress like sepsis, pregnancy, and after abdominal surgery (5-14). During this period, there is a surge of circulating catecholamines and adrenocorticotrophic hormone (ACTH) that leads to vasoconstriction of the draining venules (15). Increased platelet aggregation as a result of high level of catecholamines predispose to adrenal vein thrombosis (4). Subsequently, venous stasis and increase in adrenal venous pressure leads to rupture of the thin walled adrenal venules (3). Other conditions reported to be linked with spontaneous adrenal haemorrhage are anti-phospholipid syndrome, anticoagulant and haematological disorders (16-18).
Spontaneous adrenal haemorrhage has been defined variably in the literature. Some authors refer to this as the absence of trauma or anti-coagulant use while others restrict its use to cases where there is no obvious predisposition other than adrenal pathology (19,20). Bleeding in the absence of any adrenal pathology (i.e., normal adrenals on imaging after resolution of bleeding) and without other predisposing factors is thought to be very rare.
Literature on the management of adrenal haemorrhage is limited. In the published case reports, most patients are initially treated conservatively (5,10-14). Surgical resection has been performed electively by either the open or laparoscopic approach (9,21). CT scan may be performed during follow-up to monitor the size of the haematoma and evaluate any underlying lesion (22). Other options of treatment reported are urgent surgical resection (23) and angioembolisation of the adrenal arteries (8,23,24). However, both emergency treatments were reserved in patients with hemodynamic instability.
The objective of this study is to evaluate the clinical presentation, underlying predisposition and management strategies in adult patients who were referred to a single tertiary unit with acute abdominal pain secondary to non-traumatic adrenal haemorrhage.
Methods
This study was a retrospective review of the medical records of consecutive adult patients presented with acute adrenal haemorrhage and referred to the endocrine surgery unit at Sheffield Teaching Hospitals from 2012 to 2018. Patients who had evidence of recent bleed on radiology but did not present acutely with features consistent with bleeding and those with adrenal bleeding following trauma were excluded.
In addition to routine assessment and monitoring, computed tomography was performed in all patients at the time of the acute episode. Biochemical investigations such as serum cortisol, renin and aldosterone level and plasma or urine assessment for catecholamine/metanephrine excess were performed following resolution of the acute event.
Information on demographics, presentation, diagnosis and management was retrieved by one observer and validated by another. As this was a case series, no formal ethics application or informed patient consent was deemed necessary. Patient details were kept in secure electronic servers within the hospital intranet and the data was anonymised prior to analyses and reporting.
Results
In total, 11 patients were referred following a recent admission for spontaneous adrenal haemorrhage between 2012–2018. Of this, 7 (63.6%) patients were female and 4 (36.4%) were male. The median (range) age was 58 years (range, 27–89 years). Four (36.4%) patients were on anticoagulants (2 on rivaroxaban and 2 on warfarin) for atrial fibrillation.
Five (45.5%) patients underwent definitive surgical treatment after a median [range] of 10 [7–11] weeks. One patient who underwent surgery and another patient managed conservatively died of disseminated non-adrenal malignant disease at 5 and 2 months respectively after presentation with bleeding. Two other patients died of non-adrenal disease at 28 and 12 months after initial presentation. Conservative management in the other 3 patients was successful at a median follow up of 26 [6–66] months. Table 1 showed the summary of demographic factors, initial management and follow up of patients presenting with acute, non-traumatic adrenal haemorrhage.
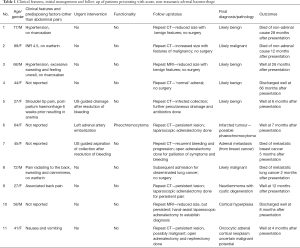
Full table
Discussion
Acute adrenal haemorrhage presents mostly with abdominal and flank pain (25,26), as noted in all our patients. Other symptoms like neuropsychiatric presentations, hypotension and anaemia are uncommon (27). A number of conditions are reported to be associated with non-traumatic adrenal haemorrhage as mentioned previously (3,5-18). Recognition of these existing predisposing factors (in particular anti-coagulant use) may help determine the initial management plan in this group of patients. In the patients on anti-coagulants in our series; bleeding appeared to resolve in all four patients.
Although pregnancy is a known risk factor for adrenal haemorrhage (10,11), the risk is unclear (28). It may occur without additional factors and is reported in complicated pregnancies such as hyperemesis gravidarum and difficult labour (11,28,29). One patient in our case series had history of post-partum haemorrhage 15 weeks before presentation.
Regardless of underlying risk factors, biochemical testing for hyperfunction and repeat cross-sectional imaging after the acute event is required to exclude underlying adrenal pathology. In a systematic review, 80% of bleeding adrenal tumours were benign (26). Common benign tumours underlying bleeding include phaeochromocytoma (15), cortical lesions, adrenal pseudo cysts and lipomas (21,30). Malignant adrenal tumours associated with adrenal haemorrhage include adrenocortical carcinoma and metastasis (26). Nevertheless, in around 13% of patients with adrenal haemorrhage, no significant underlying pathology was detected and follow up imaging demonstrated regression of the hematoma without no evidence of an underlying adrenal mass (26). In this presented case series, four patients had resolution of bleeding with either benign looking or ‘normal sized’ adrenals on repeat imaging. These four patients along with two others with adrenal metastases in the context of disseminated disease did not undergo surgery. Of those who had surgery, one had a phaeochromocytoma (n=5), the pathology included a possible phaeochromocytoma, a benign cortical lesion, a metastasis, a neurilemmoma and a lesion of uncertain malignant potential.
The definitive management of the non-traumatic adrenal haemorrhage is still uncertain and debatable. Initial conservative management has now replaced the trend of early surgery in early years due to increasing availability of CT scan (31). In patients with evidence of persistent bleeding and hemodynamic instability despite supportive care, angioembolisation has been used with good results in the acute setting (8,24). In the presented case series, angioembolisation was done in one patient and two patients required aspiration and drainage for infected hematoma soon after the acute episode.
In the systematic review, the majority of patients who presented with adrenal haemorrhage eventually had interval adrenalectomy (26). Interval adrenalectomy will allow the resolution of inflammatory process, thereby reducing the morbidity of surgery and facilitating minimally invasive approaches. In the presented case series (n=11), five patients had undergone adrenalectomy for either persistent symptoms, hyper function or indeterminate lesions on imaging. The laparoscopic approach was used in two patients, hand-assist laparoscopy in one and open approach in two.
In conclusion, initial conservative management is the preferred treatment as the surgery may be avoidable in some instances. Further investigations after resolution of bleeding will allow the clinician to determine the functional status and reassess the lesion on imaging. This will ensure that the patients are well-optimized before elective surgery and minimally invasive approaches may be used in an elective setting, if appropriate.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: As this was a case series, no formal ethics application or informed patient consent was deemed necessary.
References
- Botteri A, Orell SR. Adrenal Hemorrhage and Necrosis in the Adult. A Clinicopathological Study of 23 Cases. Acta Med Scand 1964;175:409-19. [Crossref] [PubMed]
- Plaut A. Adrenal necrosis and thrombosis in routine necropsies. Am J Pathol 1955;31:93-105. [PubMed]
- Rao RH, Vagnucci AH, Amico JA. Bilateral massive adrenal hemorrhage: early recognition and treatment. Ann Intern Med 1989;110:227-35. [Crossref] [PubMed]
- Kovacs KA, Lam YM, Pater JL. Bilateral massive adrenal hemorrhage. Assessment of putative risk factors by the case-control method. Medicine (Baltimore) 2001;80:45-53. [Crossref] [PubMed]
- Khwaja J. Bilateral adrenal hemorrhage in the background of Escherichia coli sepsis: a case report. J Med Case Rep 2017;11:72. [Crossref] [PubMed]
- Wharton J, Cohen D. Delayed Unilateral Adrenal Hemorrhage Complicating Pneumococcal Septic Shock. Del Med J 2015;87:310-2. [PubMed]
- Girgis CM, Cole L, Champion BL. Bilateral adrenal haemorrhage in a critically ill patient. Crit Care Resusc 2011;13:123-4. [PubMed]
- Laack J, Trigger C. Spontaneous Adrenal Hemorrhage in Pregnancy Presenting as a Pulmonary Embolism. J Emerg Med 2016;50:e97-8. [Crossref] [PubMed]
- Angelico R, Ciangola IC, Mascagni P, et al. Laparoscopic adrenalectomy for hemorrahagic adrenal pseudocyst discovered during pregnancy: report of a case. Surg Laparosc Endosc Percutan Tech 2013;23:e200-4. [Crossref] [PubMed]
- Bockorny B, Posteraro A, Bilgrami S. Bilateral spontaneous adrenal hemorrhage during pregnancy. Obstet Gynecol 2012;120:377-81. [Crossref] [PubMed]
- Anagnostopoulos A, Sharma S. Spontaneous adrenal haemorrhage in pregnancy. BMJ Case Rep 2011;2011.
- Sasiwimonphan K, Takahashi N, Leibovich BC, et al. Adrenal hematoma after nephrectomy. AJR Am J Roentgenol 2010;195:1334-7. [Crossref] [PubMed]
- Peel N, Whitelaw SC. Bilateral adrenal haemorrhage following right hemicolectomy. Int J Colorectal Dis 2011;26:681-2. [Crossref] [PubMed]
- Munoz Corsini L, Delgado Arnaiz C, Garcia del Valle S, et al. Postoperative bilateradddl adrenal hemorrhage: correlation between clinical and radiological signs. J Clin Anesth 2008;20:605-8. [Crossref] [PubMed]
- Kawashima A, Sandler CM, Ernst RD, et al. Imaging of nontraumatic hemorrhage of the adrenal gland. Radiographics 1999;19:949-63. [Crossref] [PubMed]
- Michon A, Darnige L, Pouchot J, et al. Catastrophic antiphospholipid syndrome presenting with bilateral massive adrenal haemorrhage. A case report. Joint Bone Spine 2015;82:288-9. [Crossref] [PubMed]
- Namias N. Chance favors the prepared mind: the association between heparin-induced thrombocytopenia and bilateral adrenal hemorrhage. Crit Care Med 2011;39:912-3. [Crossref] [PubMed]
- Kojima K, Fujii N, Takata S, et al. Bilateral adrenal hemorrhage in essential thrombocythemia. Ann Hematol 2002;81:350-1. [Crossref] [PubMed]
- Nazir S, Sivarajah S, Fiscus V, et al. Spontaneous idiopathic bilateral adrenal haemorrhage: a rare cause of abdominal pain. BMJ Case Rep 2016;2016.
- Ogino J, Toda J, Onitsuka S, et al. Idiopathic bilateral adrenal haemorrhage related to acute adrenal insufficiency. BMJ Case Rep 2013;2013.
- Geleit RJ, Bhardwaj R, Fish D, et al. A unique presentation of a complex haemorrhagic adrenal pseudocyst. BMJ Case Rep 2016;2016.
- Yamada T, Yamakawa F, Cao X, et al. Conservative Treatment for Idiopathic Adrenal Hemorrhage Tracked by a Long-term Series of CT Images. Intern Med 2017;56:673-6. [Crossref] [PubMed]
- Goldman HB, Howard RC, Patterson AL. Spontaneous retroperitoneal hemorrhage from a giant adrenal myelolipoma. J Urol 1996;155:639. [Crossref] [PubMed]
- Prabhasavat K, Ruamcharoenkiat S. Outcomes of Arterial Embolization of Adrenal Tumor in Siriraj Hospital: Case Report. J Med Assoc Thai 2015;98:621-7. [PubMed]
- Vella A, Nippoldt TB, Morris JC 3rd. Adrenal hemorrhage: a 25-year experience at the Mayo Clinic. Mayo Clin Proc 2001;76:161-8. [Crossref] [PubMed]
- Marti JL, Millet J, Sosa JA, et al. Spontaneous adrenal hemorrhage with associated masses: etiology and management in 6 cases and a review of 133 reported cases. World J Surg 2012;36:75-82. [Crossref] [PubMed]
- Tormos LM, Schandl CA. The significance of adrenal hemorrhage: undiagnosed Waterhouse-Friderichsen syndrome, a case series. J Forensic Sci 2013;58:1071-4. [Crossref] [PubMed]
- Gavrilova-Jordan L, Edmister WB, Farrell MA, et al. Spontaneous adrenal hemorrhage during pregnancy: a review of the literature and a case report of successful conservative management. Obstet Gynecol Surv 2005;60:191-5. [Crossref] [PubMed]
- Gupta A, Minhas R, Quant HS. Spontaneous Adrenal Hemorrhage in Pregnancy: A Case Series. Case Rep Obstet Gynecol 2017;2017. [Crossref] [PubMed]
- Kapetanakis S, Drygiannakis I, Tzortzinis A, et al. A giant adrenal lipoma presenting in a woman with chronic mild postprandial abdominal pain: a case report. J Med Case Rep 2011;5:136. [Crossref] [PubMed]
- Simon DR, Palese MA. Clinical update on the management of adrenal hemorrhage. Curr Urol Rep 2009;10:78-83. [Crossref] [PubMed]


