The evolution of mastectomies in the oncoplastic breast surgery era
Introduction
Over time, surgical techniques have advanced to the point where oncological safety and aesthetic outcomes are the pillars of contemporary breast surgery. Although can a mastectomy be considered an oncoplastic surgical procedure? Can this procedure be called “oncoplastic mastectomy”? Can it be included in the arsenal against breast cancer? To answer those questions it is important to understand part of the evolution of breast cancer surgical treatment.
The partial evolution of treatment
Oncoplastic surgery
By the early 90’s Audretsch (1) suggested the integration of plastic surgery techniques with breast-conserving treatment (BCT) for breast cancer. Conceptually, this approach was referred as “oncoplastic surgery”, which aims at providing safe oncologic treatment through careful pre-operative planning and the incorporation of plastic surgery techniques in order to obtain good oncologic control with favorable cosmetic results in cases of large breast volume and large tumors. Subsequently the concept was accorded the term tumour specific immediate reconstruction. Moreover, oncoplastic surgery very often offers improved overall aesthetic outcomes and favors the achievement of contralateral breast symmetry (2).
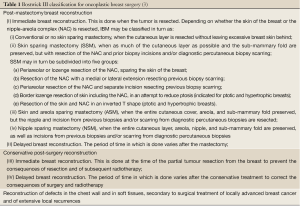
The american plastic surgeon John Bostwick III in 1996, suggested that the term Oncoplastic Breast Surgery (OBS) includes not only techniques preventing the consequences of conservative treatment but also a whole range of techniques involving partial or total immediate post-mastectomy reconstruction (immediate breast reconstruction), correction of their consequences (delayed breast reconstruction), and immediate repair of the surgical treatment of locally advanced tumours and recurrences in the chest wall. Nowadays, following a period of uncertainty in the nomenclature, the term OBS is uniformly associated in the medical community with the classification system of John Bostwick III (Table 1), in both Latin and Anglo-Saxon publications (3). It is important to clarify that the term OBS also encompasses the techniques developed for preventive surgery in high-risk patients (risk reduction mastectomies).
Skin sparing mastectomy
Down this same path, the mastectomy has changed and Toth & Lappert (4) described the Skin Sparing Mastectomy technique (SSM) in association with the removal of malignant tumors. It allowed the conservation of a large part of the skin and mammary fold in favor of immediate breast reconstruction (IBR).
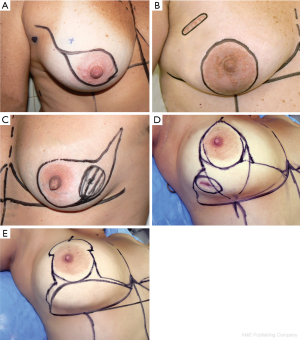
Carlson et al. (5) considered four different types of incisions for SSM (Figure 1). The incision type IV is an example of using a plastic surgery technique to perform mastectomy. It is called Wise-pattern skin sparing mastectomy (WPM) which enabled excellent results as IBR in heavy and pendulous-breasted patients who require a conspicuous reduction of the skin envelope and a contralateral reduction or mastopexy. However, the side undergoing the WPM, the skin flaps are thin and wound healing problems are well described, particularly skin necrosis at the “T” as frequent as 27%, predisposing to prosthesis exposure and therefore limiting its utility. Thus, Nava et al. (6) described a modification of this last type of skin-sparing mastectomy, that he called skin-reducing mastectomy. In that case the mammary reconstruction in selected patients is performed in a single-stage in which an anatomical silicone gel implant is placed in a dermal muscle flap pocket. It also allows the achievement of contralateral breast symmetry (Figures 2,3).
Nipple sparing mastectomy (NSM)
Other variations of mastectomy came up and started allowing the oncological safety and the possiblity of an IBR. Defending the idea of IBR performed by breast surgeons trained in oncoplastic surgery or by dedicated teams of breast surgeons and reconstructive surgeons, Petit et al. (7), described the nipple-sparing mastectomy as an option for patients with small invasive and non-invasive cancer located far from the nipple-areola complex. The principle of complete removal of breast gland with preservation of skin and also nipple-areola complex was maintained. At the beginning it was indicated in small breast women with multicentric disease, extensive intraductal carcinoma and especially when there was an unfavorable relation between breast volume and tumor size and also for women at high risk.
Risk-reducing mastectomy (RRM)
It is important to mention the prophylactic mastectomy or RRM responsable for sparing the most part of skin and nipple areola-complex but it is indicated for benign treatment or for reducing cancer risk. It has been largely performed for patients displaying the following oncologic risk factors: a positive family history, BRCA-1 and -2 gene mutation, atypic ductal hyperplasia, intensive lobular carcinoma in situ, and ductal carcinoma in situ and still when an extreme fear of breast cancer is manisfested. RRM has been performed increasingly due to either patient demand or oncologic surgeon proposal. Sparing of the nipple-areola complex is extremely important for aesthetic results and patient satisfaction in both early-stage breast cancer and high-risk groups.
Conservative mastectomy
Nowadays the principle of oncoplastic surgery is amplified and was incorporated to the idea of an IBR. Recently Veronesi et al. (8) published the term conservative surgery regarding a surgical technique demanding on an oncological treatment by removing the breast parenchyma and trying to spare as much skin envelope as possible, including nipple areolar complex. In other words to remove breast glandular tissue without disruption of the breast appearance. It allows an IBR and the contralateral symmetric approach. It also boosts the patient’s self-esteem and quality of life.
Conclusions
There are no doubts that mastectomy remains the most common choice of treatment for breast cancer around the world. More often the patients, especially young women, are looking for a safety oncological treatment warranted by the benefits of breast reconstruction. The breast surgical procedures were updated and the mastectomy too. Those modalities of mastectomy are safe techniques providing better cosmetic outcome without compromising oncological safety as per the current evidence (9). They have allowed the approach of large tumors with an IBR something regarded as unthinkable in the past (10). Moreover the recent literature showed that IBR is a feasible and safe option for women undergoing mastectomies for their breast cancer (9). Today it is important to individualize each case, listen to the patient, clarify her doubts and try to provide the best option for each situation. It is also important to explain the risks of complications and delays to adjuvant therapy. Although radiotherapy does not represent a contraindication to IBR there is no consensus about the adjuvant treatment.
In short, the mastectomy with IBR is one of the best alternatives to treat breast cancer and also the most suitable solution to the relevant points of body image if well indicated. This manuscript does not defend the indiscriminate use of mastectomy but the idea to create and use the term “oncoplastic mastectomy” to the different kinds of sparing mastectomies. It can definitely be used as an evolutionary weapon against breast cancer.
Acknowledgements
A special thank to Mr Wilson Marçal for proofreading the manuscript. We also appreciate the cooperation of all colleagues in the Breast Unit-Barretos Cancer Hospital.
Disclosure: The authors declare that they have no commercial competing interests or financial support for this study.
References
- Audretsch W, Rezai M, Kolotas C, et al. Onco-plastic surgery: “Target” volume reduction (BCT-mastopexy), lumpectomy, reconstruction (BCT-reconstruction), and flap-supported operability in breast cancer. Second European Congress on Senology, Breast Diseases 1994:139-57.
- Clough KB, Lewis JS, Couturaud B, et al. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg 2003;237:26-34. [PubMed]
- Rancati A, Gonzalez E, Dorr J, et al. Oncoplastic surgery in the treatment of breast cancer. Ecancermedicalscience 2013;7:293. [PubMed]
- Toth BA, Lappert P. Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning. Plast Reconstr Surg 1991;87:1048-53. [PubMed]
- Carlson GW, Bostwick J 3rd, Styblo TM, et al. Skin-sparing mastectomy. Oncologic and reconstructive considerations. Ann Surg 1997;225:570-5. [PubMed]
- Nava MB, Cortinovis U, Ottolenghi J, et al. Skin-reducing mastectomy. Plast Reconstr Surg 2006;118:603-10. [PubMed]
- Petit JY, Veronesi U, Orecchia R, et al. Nipple-sparing mastectomy in association with intra operative radiotherapy (ELIOT): A new type of mastectomy for breast cancer treatment. Breast Cancer Res Treat 2006;96:47-51. [PubMed]
- Veronesi U, Stafyla V, Petit JY, et al. Conservative mastectomy: extending the idea of breast conservation. Lancet Oncol 2012;13:e311-7. [PubMed]
- Piper M, Peled AW, Foster RD, et al. Total skin-sparing mastectomy: a systematic review of oncologic outcomes and postoperative complications. Ann Plast Surg 2013. [Epub ahead of print]. [PubMed]
- Zucca Matthes AG, Uemura G, Kerr L, et al. Feasibility of oncoplastic techniques in the surgical management of locally advanced breast cancer. Int J Surg 2012;10:500-5. [PubMed]