Liver transplantation for unresectable pancreatic neuroendocrine tumors with liver metastases in an era of transplant oncology
Introduction
Pancreatic neuroendocrine tumors (pNETs) represent approximately 7% of all NETs. Their prevalence has considerably increased over the last three decades, which is primarily due to improvements in imaging and diagnostic techniques (1,2). Despite the increased diagnosis of incidental lesions, 40–95% of patients present with a metastatic disease at the first diagnosis (2,3). Liver metastases (LM) develop in more than 50% of patients with pNETs, which strongly influences their prognosis (3,4). Accumulated experience indicates a worse 5-year overall survival rate for metastatic pNETs (40–60%) than that for metastatic intestinal NETs (56–83%) (3).
The conventional treatment of metastatic pNETs involves a combination of surgical resection (5), systemic chemotherapy, liver-directed therapies such as transarterial chemoembolization and radiofrequency ablation. More recently, peptide receptor radionuclide therapy (6) and molecular-targeted therapy such as sunitinib (7) and everolimus (8) have emerged as novel approaches and have substantially improved the survival rate for pNETs (9). Although liver transplantation (LT) for unresectable pNET with liver metastases (pNETLM) has been described to prolong survival in highly selected patients, most of the data do not reflect the improvements of non-surgical treatments. Therefore, the role of LT should be reconsidered. A new era of “Transplant Oncology” has begun, and we stand at the dawn of a paradigm shift in multidisciplinary treatment for metastatic pNETs (10). In this review, the current status and future role of LT as a treatment for pNETLM are discussed in the context of transplant oncology.
Most previous reports that have evaluated the efficacy of LT as a treatment for NETLM have been single-center studies based on limited number of cases. Recently, there have been efforts to collect large dataset by multi-center studies or to analyze registry databases. However, these studies were conducted either in the United States or in Europe, and prospective trials are extremely rare in this field; thus, the generalizability of their results remains questionable.
Proposed criteria and controversies
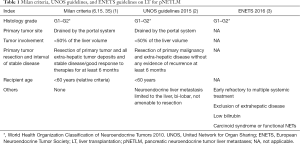
Patients who undergo LT for NETLM need to be carefully selected with certain criteria to effectively use grafts in the face of a critical shortage of organs. Several proposed criteria are described in this review with their rationale and controversies, including the European Neuroendocrine Tumor Society (ENETS) guidelines, the Milan criteria, and the United Network for Organ Sharing (UNOS) guidelines.
ENETS guidelines
The ENETS consensus guidelines 2016 states that LT for NETLM is generally not recommended but may be an option in highly selected patients with carcinoid syndrome or other functional NETs and diffuse liver disease, early refractory to multiple systemic treatments, locoregional therapies, and peptide receptor radionuclide therapy (3). They conclude that the precise preselection of patients (e.g., G1/G2 NET, exclusion of extrahepatic disease, and low bilirubin) for LT may further improve survival rates (11-13).
The European Liver Transplant Registry database analysis, which incorporated a total of 213 patients with NETLM, noted 1-, 3-, 5-year survival rates of 81%, 65%, and 52%, respectively (14). Le Treut et al. have reported that patients with pNETs had a worse 5-year survival rate than patients with gastrointestinal NETs (GI-NETs) (44% vs. 62%, respectively; P<0.05). In 40% of the patients who underwent LT for pNETLM, the cause of death was the recurrent disease at a median delay of 52 months after LT (range, 4–165 months) (14). Le Treut et al. have identified a number of important prognostic factors associated with worse long-term survival, including the resection of the primary tumor during LT and the presence of hepatomegaly, LT with >50% of liver tumor involvement, and tumor bulk as the primary indication for LT. In addition, poorly differentiated tumors, margin-positive resection, and lymph node-positive disease were all associated with worse long-term survival (14).
A French multi-center study has reported similar survival rates for pNETLM and GI-NETLM (27% vs. 69%, respectively, P=0.0008) (15). In another study, data suggested that both 1-year overall survival rate and 1-year disease-free survival rate for pNETLM were inferior to those for GI-NETLM; however, the difference was not statistically significant probably due to small sample size (77% vs. 100%, P=0.2 and 60% vs. 100%, P=0.1, respectively) (16).
Milan criteria
The Milan criteria were developed at the National Cancer Institute of Milan in 1995 (17). The criteria are described in detail in Table 1. In their prospective study, Mazzaferro et al. have reported a remarkable 5-year OS rate for NETLM patients treated with LT (97.2%) compared to that for patients treated with a non-transplant strategy (50.9%) (18). The study also suggested that transplant-related survival benefit increased over time, maximizing at 10 years after LT (10-year OS rate, 88.8% vs. 22.4%). However, some patients selected according to these strict criteria may not have required LT (15), whereas some patients who were excluded from LT may still have enjoyed long-term survival.
Full table
UNOS guidelines
The UNOS has published guidelines regarding the evaluation of patients with NETLM for whom excellent outcomes after LT can be achieved when strict selection criteria are applied (19). Based on the UNOS database from 2002–2014, Nobel et al. have reported 1-, 3-, 5-year OS rates of 89%, 69%, and 63%, respectively (13). The UNOS guidelines are based on the results of several studies (14,15) in Europe, including a study underlying the Milan criteria (17); thus, the UNOS guidelines is similar to the Milan criteria (Table 1). The guidelines state an inclusion criterion of resection of primary malignancy and extra-hepatic disease without any evidence of recurrence for at least 6 months, which differs from that in the Milan criteria of stable disease or response to therapies for at least 6 months. Although these two guidelines include a delay of at least 6 months to assess tumor progression, this was arbitrarily selected as an inclusion criterion in a study by Mazzaferro (18). However, the association between this criterion and the remarkable results of this study lacked a robust evidence. A previous report has suggested that a patient would have a better outcome after LT if the liver lesion from metastatic NETs took a long time to evolve (20). Currently, many physicians have a perception that asymptomatic patients with stable diseases may not require LT, whereas patients with progressive diseases refractory to non-surgical treatment may require LT (12). However, there is no evidence to permit any strong conclusion in this respect. The timing of LT for NETLM should be reconsidered after further prospective studies focusing on the timing of LT.
In contrast, the National Comprehensive Cancer Network guidelines version 2.2017 deemed LT to be investigational and not a part of routine care on the basis of results of a meta-analysis that revealed better 5-year survival rates; however, the majority of patients who underwent LT ultimately developed recurrence (21).
Among the studies regarding LT for NETLM, a few reports have discussed outcomes stratified by the primary tumor site (14-16). Outcomes of patients who underwent LT for pNETLM were worse than those of patients who underwent LT for GI-NETLM. A review including 20 studies encompassing 89 patients who underwent LT for pNETLM has reported cumulative 1-, 3-, and 5-year survival rates of 71%, 55%, and 44%, respectively. The calculated median survival rate was 41 months (22). One of the reasons for poor outcomes of patients with LT for pNETLM may be that in most cases of pNETs, the disease has already progressed by the time treatment is started. Another reason may relate to LT with simultaneous pancreatic resection. Addition of a highly invasive surgical procedure to LT and the absence of a wait time to clearly determine the biological behavior of the primary tumor may have led to worse prognoses. Moreover, Máthé et al. have indicated a recipient age of ≥55 years (P=0.0262) and LT with simultaneous pancreatic resection (P=0.0143) as significant negative predictors (22). There have been no prospective studies that have stratified treatment outcomes by primary tumor site. Such a study is required to evaluate the efficacy of LT for pNETLM.
Future directions
Number of studies have reported prognostic factors to establish appropriate LT selection criteria and improve long-term outcomes of LT for NETLM (13-15,17,23-26). However, previous reports included either no case or only a few cases that were treated with newly developed molecular-targeted agents such as sunitinib and everolimus. They play a critical role in the treatment of advanced pNETs (7,8) and should be considered for refinement or expansion of the currently proposed criteria. Furthermore, immunosuppression after LT may increase the risk of disease recurrence. A randomized trial was conducted recently to investigate the clinical implication of sirolimus, an antineoplastic immunosuppression, in LT recipients with hepatocellular carcinoma. Although the study failed to meet its primary endpoint, it did show some survival benefit in a subset of low-risk patients (27). Everolimus is a derivative of sirolimus and they both belong to the same class of immunosuppressants by inhibition of the mammalian target of rapamycin. Properly designed studies are necessary to define the role of down-staging and bridging therapy prior to LT incorporating systemic chemotherapy using molecular-targeted agents, locoregional treatments, and peptide receptor radionuclide therapy, and optimal immunosuppression protocol after LT with antineoplastic immunosuppression.
Another clinical question is: What is an appropriate measurement outcome of treatment for NETLM? Given the indolent nature of low or intermediate grade pNETs, the best endpoint (overall survival, disease-free survival, relapse-free survival, progression-free survival, etc.) to compare the efficacy of each treatment option for patients with pNETLM has yet to be determined. The upcoming WHO 2017 classification of pNETs also needs to be taken into consideration (28).
Lastly, the definition of “unresectable” remains ambiguous. The indication of the conventional technique of two-staged liver resection with portal vein embolization or the rapidly spreading new technique of associating liver partition and portal vein ligation for staged hepatectomy to expand the resectability of wide-spread metastatic liver tumors has been controversial. In an era of transplant oncology, LT should be the last resort for patients who are considered unresectable and otherwise untreatable after an exhaustive multidisciplinary team discussion with all aggressive surgical and medical options on board (29).
Conclusions
Although its long-term outcomes have been promising under several proposed criteria, the role of LT for unresectable pNETLM as a curative or palliative treatment remains unclear. The development of molecular-targeted agents has changed the landscape of treatment for pNETs. Moreover, the dispute over the definition of “unresectable” LM has yet to be settled. Ultimately, a well-designed randomized control study is required to elucidate the clinical impact of LT for pNETLM.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cidon EU. New therapeutic approaches to metastatic gastroenteropancreatic neuroendocrine tumors: A glimpse into the future. World J Gastrointest Oncol 2017;9:4-20. [Crossref] [PubMed]
- Orditura M, Petrillo A, Ventriglia J, et al. Pancreatic neuroendocrine tumors: Nosography, management and treatment. Int J Surg 2016;28:S156-62. [Crossref] [PubMed]
- Frilling A, Modlin IM, Kidd M, et al. Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol 2014;15:e8-21. [Crossref] [PubMed]
- Steinmuller T, Kianmanesh R, Falconi M, et al. Consensus guidelines for the management of patients with liver metastases from digestive (neuro)endocrine tumors: foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 2008;87:47-62. [Crossref] [PubMed]
- Hibi T, Sano T, Sakamoto Y, et al. Surgery for hepatic neuroendocrine tumors: a single institutional experience in Japan. Jpn J Clin Oncol 2007;37:102-7. [Crossref] [PubMed]
- Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 Trial of (177) Lu-Dotatate for Midgut Neuroendocrine Tumors. N Engl J Med 2017;376:125-35. [Crossref] [PubMed]
- Raymond E, Dahan L, Raoul JL, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med 2011;364:501-13. [Crossref] [PubMed]
- Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med 2011;364:514-23. [Crossref] [PubMed]
- Lee L, Igarashi H, Fujimori N, et al. Long-term outcomes and prognostic factors in 78 Japanese patients with advanced pancreatic neuroendocrine neoplasms: a single-center retrospective study. Jpn J Clin Oncol 2015;45:1131-8. [PubMed]
- Hibi T, Itano O, Shinoda M, et al. Liver transplantation for hepatobiliary malignancies: a new era of "Transplant Oncology" has begun. Surg Today 2017;47:403-15. [Crossref] [PubMed]
- Pavel M, O'Toole D, Costa F, et al. ENETS consensus guidelines update for the management of distant metastatic disease of intestinal, pancreatic, bronchial neuroendocrine neoplasms (NEN) and NEN of unknown primary site. Neuroendocrinology 2016;103:172-85. [Crossref] [PubMed]
- Fan ST, Le Treut YP, Mazzaferro V, et al. Liver transplantation for neuroendocrine tumour liver metastases. HPB (Oxford) 2015;17:23-8. [Crossref] [PubMed]
- Nobel YR, Goldberg DS. Variable use of model for end-stage liver disease exception points in patients with neuroendocrine tumors metastatic to the liver and its impact on patient outcomes. Transplantation 2015;99:2341-6. [Crossref] [PubMed]
- Le Treut YP, Grégoire E, Klempnauer J, et al. Liver transplantation for neuroendocrine tumors in Europe-results and trends in patient selection: a 213-case European liver transplant registry study. Ann Surg 2013;257:807-15. [Crossref] [PubMed]
- Le Treut YP, Grégoire E, Belghiti J, et al. Predictors of long-term survival after liver transplantation for metastatic endocrine tumors: an 85-case French multicentric report. Am J Transplant 2008;8:1205-13. [Crossref] [PubMed]
- van Vilsteren FG, Baskin-Bey ES, Nagorney DM, et al. Liver transplantation for gastroenteropancreatic neuroendocrine cancers: Defining selection criteria to improve survival. Liver Transpl 2006;12:448-56. [Crossref] [PubMed]
- Mazzaferro V, Pulvirenti A, Coppa J. Neuroendocrine tumors metastatic to the liver: how to select patients for liver transplantation? J Hepatol 2007;47:460-6. [Crossref] [PubMed]
- Mazzaferro V, Sposito C, Coppa J, et al. The long-term benefit of liver transplantation for hepatic metastases from neuroendocrine tumors. Am J Transplant 2016;16:2892-902. [Crossref] [PubMed]
- OPTN. Guidanse on MELD PELD exception review. Organ Procurement and Transplantation Network. 2015. Available online: https://optn.transplant.hrsa.gov/resources/by-organ/liver-intestine/guidance-on-meld-peld-exception-review/#NET
- Gedaly R, Daily MF, Davenport D, et al. Liver transplantation for the treatment of liver metastases from neuroendocrine tumors: an analysis of the UNOS database. Arch Surg 2011;146:953-8. [Crossref] [PubMed]
- Rossi RE, Burroughs AK, Caplin ME. Liver transplantation for unresectable neuroendocrine tumor liver metastases. Ann Surg Oncol 2014;21:2398-405. [Crossref] [PubMed]
- Máthé Z, Tagkalos E, Paul A, et al. Liver transplantation for hepatic metastases of neuroendocrine pancreatic tumors: a survival-based analysis. Transplantation 2011;91:575-82. [Crossref] [PubMed]
- Le Treut YP, Delpero JR, Dousset B, et al. Results of liver transplantation in the treatment of metastatic neuroendocrine tumors. A 31-case French multicentric report. Ann Surg 1997;225:355-64. [Crossref] [PubMed]
- Frilling A, Malago M, Weber F, et al. Liver transplantation for patients with metastatic endocrine tumors: single-center experience with 15 patients. Liver Transpl 2006;12:1089-96. [Crossref] [PubMed]
- de Herder WW, Mazzaferro V, Tavecchio L, et al. Multidisciplinary approach for the treatment of neuroendocrine tumors. Tumori 2010;96:833-46. [PubMed]
- Sher LS, Levi DM, Wecsler JS, et al. Liver transplantation for metastatic neuroendocrine tumors: Outcomes and prognostic variables. J Surg Oncol 2015;112:125-32. [Crossref] [PubMed]
- Geissler EK, Schnitzbauer AA, Zülke C, et al. Sirolimus use in liver transplant recipients with hepatocellular carcinoma: a randomized, multicenter, open-label phase 3 trial. Transplantation 2016;100:116-25. [Crossref] [PubMed]
- Kim JY, Hong SM, Ro JY. Recent updates on grading and classification of neuroendocrine tumors. Ann Diagn Pathol 2017;29:11-6. [Crossref] [PubMed]
- Schaefer B, Zoller H, Schneeberger S. Con: Liver transplantation for expanded criteria malignant diseases. Liver Transpl 2018;24:104-11. [Crossref] [PubMed]


