The PGRIS and parathyroid splinting concepts for the analysis and prognosis of protracted hypoparathyroidism
Introduction
Hypocalcemia due to acute parathyroid failure is observed in 20–60% of the patients undergoing total thyroidectomy of whom 1–10% will develop permanent hypoparathyroidism (1,2). Such wide variation is due to multiple factors such as definitions used, precision in data gathering, conflicts of interest, surgical expertise, lymph node dissection and parathyroid preservation vs. autotransplantation policies.
Patients with postoperative hypocalcemia (<8 mg/dL or 2 mmol/L at 24 h) or hypoparathyroidism [parathyroid hormone (PTH) <10–15 pg/mL at 4–6 h] are discharged home on calcium and calcitriol and about two thirds will show a normal parathyroid function within the following 3–6 weeks. We are starting to understand why 20–30% of patients with postoperative parathyroid failure will require prolonged replacement therapy after this time interval and also the factors influencing recovery of the parathyroid function after a more or less prolonged period of medical treatment (even after 1-year follow-up). This is what this article is about. It is hoped that it will help the reader to better understand the causes of protracted postoperative parathyroid insufficiency and to provide new clues for an improved technical performance when practicing extensive thyroid surgery. The definitions of the different parathyroid failure syndromes put forward by our team will be used throughout the present narrative article in which we will discuss some emerging concepts related to post-thyroidectomy hypoparathyroidism (3).
PGRIS: a clue to understand prolonged parathyroid failure
Several demographic, disease-related and surgical variables have been implicated—through different mechanisms—in the pathogenesis of postoperative hypocalcemia (Table 1). Studies on intact PTH (iPTH) kinetics shortly after thyroidectomy, however, have shown that parathyroid insufficiency is the final common pathway leading to hypocalcemia and the most relevant (if not the only) factor influencing serum calcium concentration immediately after total thyroidectomy (4,5). There is no satisfactory and agreed explanation for why about two thirds of patients will soon recover the parathyroid function whereas the rest will go on to suffer from protracted hypoparathyroidism requiring replacement therapy for more than a month. Here is where the number of parathyroid glands remaining in situ (PGRIS) concept has been particularly helpful in providing a tool to analyze the failure to recover early from postoperative hypocalcemia (6).
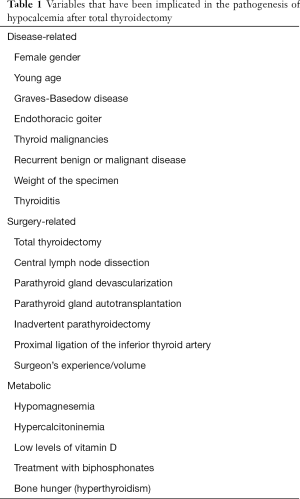
Full table
Parathyroid autotransplantation
Normal parath yroid gland autotransplantation during total thyroidectomy has been used for decades in the belief that it can prevent permanent hypoparathyroidism (7). Some authors did even suggest that it should be carried out routinely to ensure long-term parathyroid function (8,9). On the other hand, most reports investigating the short-term effects of autotransplantation have shown that it significantly increases the prevalence of postoperative hypocalcemia (8,10). Proponents of a liberal autotransplantation policy, however, argue that this short-term inconvenient is overcome by the fact that after several weeks the transplant will take and start to function thus preventing permanent hypoparathyroidism. The evidence in favor of this hypothesis is very week, at best, as shown by recent reports expressing a word of caution on the long-term outcome of autotransplantation (11-14).
Inadvertent parathyroidectomy
Incidental parathyroidectomy has received a renewed attention in the last years. It has been made clear that some 10–30% of total thyroidectomy specimens harbor inadvertently excised parathyroid glands, particularly when combined with therapeutic central neck dissection for thyroid cancer (15,16). The first reports did underestimate the influence of inadvertent parathyroid gland excision on parathyroid failure (17-20). More recent studies, however, with large series of truly total thyroidectomies carefully followed up and appropriate definitions have demonstrated that inadvertent parathyroidectomy is associated with both, postoperative short- and long-term parathyroid failure (6,15,16,21-23).
Development of the PGRIS concept.
It makes sense that autotransplantation and inadvertent parathyroid gland excision have been shown to be associated with postoperative hypocalcemia since they both reduce the amount of functioning parathyroid parenchyma left after thyroidectomy. According to data from our unit, the short and long-term impact of both events are similar. Patients with three glands preserved in situ fared the same whether the fourth gland had been autotransplanted or inadvertently excised (14). A similar experience has been reported by Tartaglia et al. (13). Thus, it was logical that we proposed to combine both events in a single concept: the number of PGRIS (6). PGRIS is easily calculated by substracting the number of parathyroid glands inadvertently excised and identified by the pathologist or autografted, from 4, the number of whole parathyroid glands found in normal anatomy. Thus:
PGRIS = 4− (PG autografted + PG incidentally removed)
Accordingly, the PGRIS group (or category) in which patients may be included in, goes from 0 (very unlikely!) to 4 (not that easy to accomplish!), and can be calculated as soon as the pathology report is available. It is recommended that the PGRIS group should be incorporated into the patients’ clinical records to better understand the evolution and long-term outcome of postoperative hypocalcemia.
PGRIS categories are closely related to the prevalence of the different parathyroid failure syndromes. In the initial publication (6) a total of 657 total thyroidectomies were included; 43 fell into PGRIS group 1–2, 186 in group 3 and 428 in group 4. The prevalence of postoperative hypocalcemia, and of protracted and permanent hypoparathyroidism was inversely related to the PGRIS group. In addition, serum calcium concentration at 24 h and iPTH concentrations at 24 h and 1 month after surgery were inversely correlated also with the PGRIS score (Table 2).

Full table
Limitations of the PGRIS concept
The functionality of in situ remaining glands
The fact that in ours and other authors’ experience (24) the prevalence of permanent hypoparathyroidism in PGRIS 4 patients is in the 2–3.5% range, indicates that the parathyroid function not only depends on PGRIS but on the functionality of the remaining glands. Thus, hypoparathyroidism may be due to non-functioning in situ preserved glands, resulting most probably from devascularization and ischemic necrosis. Visual scores for parathyroid damage correlate pretty well with postoperative metabolic parameters and suggest that surgeons can assess quite precisely the viability of the parathyroid glands (10,24,25). Initial studies with indocyanine green fluorescent angiography suggest that parathyroid vascularisation can be accurately assessed at the end of thyroidectomy (26). It is still unknown, however, if a snapshot of parathyroid vascular supply taken at the time of wound closure will reflect truly the long-term blood supply to the parathyroid glands and predict the final parathyroid status. In addition, non-identified in situ preserved parathyroid glands may obscure the potential correlation of angiography with both short- and long-term parathyroid function. Lang et al. (27) have recently warned against aggressive identification of all parathyroid glands as this may increase the prevalence of hypoparathyroidism. In their study, patients in whom four parathyroid glands were identified had less PGRIS and fared worse. Although no data are reported concerning parathyroid autotransplantation, it can be deducted that worse outcome in this group of patients was the result of a higher rate of parathyroid autografting. We were not able to reproduce Lang et al.’s (27) findings perhaps due to a more restrictive policy of parathyroid autotransplantation (6).
How careful and experienced is your pathologist?
Because PGRIS includes the parathyroid glands found within or on the resected thyroid gland by the pathologist, it seems particularly relevant that the study of the surgical specimen should be done by an experienced pathologist. Failure to identify inadvertently excised glands may induce inappropriate optimism regarding the recovery of the parathyroid function in case the patient develops postoperative hypocalcemia. Inadvertent parathyroidectomy may be considered to a certain extent as a quality criterion for thyroid surgery thus emphasizing the need for a thorough pathological investigation of the thyroidectomy and central lymphadenectomy (16) specimens.
Supernumerary glands
According to the anatomical study of Akerström et al. (28), a supernumerary gland weighing >5 mg could be found in 5% of the dissected necks usually close or within the thyro-thymic ligament. Thus, in some patients the PGRIS category may not reflect precisely the amount of the remaining parathyroid parenchyma. This may be particularly relevant for low PGRIS categories [1 and 2] since supernumerary glands may palliate the effect of loss of two or three glands. It has been reported that thymectomy increases the risk of postoperative hypocalcemia (16,29) meaning that surgeons should be particularly careful to avoid damaging or resecting this anatomical structure when approaching the lower pole of the thyroid, particularly when performing a central neck dissection for thyroid cancer.
Delayed serum calcium concentration as a key variable influencing recovery from protracted hypoparathyroidism
PGRIS is a key concept to understand why some patients develop protracted hypoparathyroidism. Once this stage is reached, however, two other variables emerge as powerful predictors of the long-term parathyroid function: the delayed serum calcium concentration and whether iPTH is undetectable or low but detectable (4–13 pg/mL) (Table 3). Because the latter cannot be modified, attention has been paid to the fact that normal-high serum calcium concentration at one postoperative month predicts a favorable outcome.

Full table
Two retrospective studies have brought to light the positive prognostic value of delayed normal-high serum calcium concentrations. Pattou et al. (30) conducted a retrospective study of a heterogeneous group of partial and total thyroidectomies, and reported that there was a high risk for permanent hypoparathyroidism if fewer than three parathyroid glands were preserved in situ during surgery, the early serum PTH level was <13 pg/mL or the “delayed” (no time interval specified) serum calcium levels were ≤8 mg/dL, under replacement therapy. Sitges-Serra et al. (23) showed a significant difference in serum calcium concentrations at one postoperative month between patients with protracted hypoparathyroidism who ultimately recovered or did not recover the parathyroid function. The first had a mean serum calcium concentration of 9.3±1 mg/dL whereas it was 8.1±1 mg/dL (P<0.001) in patients who developed permanent hypoparathyroidism, well along Pattou et al.’s (30) findings. We have been able to reproduce these results in a larger series of total thyroidectomy patients and in a prospective multicenter observational study (unpublished results). In addition, we also found that there was a synergistic positive effect of serum calcium and PGRIS (Figure 1). In summary, a high-normal serum calcium concentration and detectable PTH at one postoperative month, interact synergistically to determine the chances of recovery from protracted hypoparathyroidism.

The parathyroid splinting concept
In this section, I will try to answer the following two questions related to the influence of serum calcium concentration on long-term restoration of the parathyroid function:
- Which factors do influence serum calcium concentration in patients on replacement therapy for post-thyroidectomy hypocalcemia?
- Why does a delayed normal-high serum calcium concentration predict a favorable outcome for patients with protracted hypoparathyroidism?
Using Occam’s razor approach, it was felt that the most relevant variable determining delayed serum calcium concentrations was the calcium salts and calcitriol dosages prescribed at the time of hospital discharge. In a first study (23), replacement therapy was found to be significantly more intensive in patients who recovered from protracted hypoparathyroidism: they were prescribed 0.5 g/day more calcium element and 0.25 mcg/day more of calcitriol (Table 3). A complementary/alternative explanation (see below) is that there may be a iPTH influence since iPTH was more often detectable in patients with a good outcome and this could modulate serum calcium concentration. The identical values for phosphate concentration, however, imply that the metabolic effect of PTH was similar in both groups.
Concerning the issue of the positive influence of normal-high serum calcium concentration, we have put forward the hypothesis that this may favor restoration of the parathyroid function by inducing parathyroid metabolic rest after intraoperative injury (parathyroid splinting). Calcitriol per se can also contribute to parathyroid rest since it inhibits PTH synthesis by strongly binding to the parathyroid cell vitamin D receptor (31). We have preliminary evidence that calcitriol serum levels—and not only calcium concentration—are actually higher in patients with protracted hypoparathyroidism recovering the parathyroid function. On the other hand, hypocalcemia would have an opposite stimulating effect by inducing PTH synthesis and secretion from injured/ischemic parathyroid glands, thus increasing the oxygen demands that cannot be met by a compromised blood supply. Resting the injured parathyroid parenchyma would fit with the usual strategies used to support failing/ischemic organs such as the kidney (dialysis) or small bowel (parenteral nutrition).
Limitations of the parathyroid splinting concept
An obvious argument against the potential benefit of keeping the serum calcium concentration in the upper range of normal is that by doing so we spuriously blunt iPTH release. These patients would not have low iPTH levels because of protracted hypoparathyroidism but because intensive medical treatment would inhibit iPTH secretion from normally functioning parathyroid glands. Seminal pioneering studies did show that increasing extracellular ionized calcium up to 1.2 mmol/L (which would correspond approximately to a total serum calcium of 2.35 mmol/L or 9.5 mg/dL) results in a decrease of both iPTH excretion and synthesis both in dispersed parathyroid cells and in vivo in normal human subjects (32,33) (Figure 2). Further studies in normal volunteers (34-36) have confirmed an ionized serum calcium concentration of around 1.17 mmol/L as the set point for 50% reduction of PTH secretion; this corresponds approximately to a total serum calcium concentration of 9.3 mg/dL which fits well with the mean serum calcium concentration recorded in protracted hypoparathyroidism patients who recovered the parathyroid function (9.1 mg/dL). In these studies, a close sigmoid correlation was found between PTH release and ionized serum calcium concentration but this could not be found in our patients (R=0.119) suggesting that low iPTH was a true event and not the result of calcium suppression.
On the other hand, the calcium concentration able to modulate PTH release reported in the above discussed studies, would support the concept of parathyroid splinting since raising the serum calcium concentration through intensive replacement therapy would significantly reduce PTH secretion and thus, reduce oxygen demands from the failing/injured parathyroid glands. Further studies are needed to clarify this ambiguous physiological situation
Conclusions
Careful observational prospective research published in the last three years estimates that about 1 to 2 in 10 patients with acute post-thyroidectomy parathyroid failure will develop permanent hypoparathyroidism (6,24,37-39). The three more relevant factors influencing negatively the long-term parathyroid function are fewer PGRIS, undetectable PTH at 1 month and a low serum calcium concentration during the first weeks after thyroidectomy. Devascularization and ischemic necrosis may impair the function of the remaining parathyroid parenchyma. Autotransplantation of normal parathyroid tissue seems not to be the final answer to the problem of permanent hypoparathyroidism and it cannot be conceptually equaled to autografting of hyperplastic parathyroid glands. Surgeons should be encouraged to improve their technical performance by avoiding inadvertent parathyroidectomy and preserving the parathyroid gland blood supply (40) particularly when practicing extensive surgery for big goiters and thyroid malignancies. While further studies need to be done, current data suggest that aggressive medical therapy of post-thyroidectomy hypocalcemia may enhance the restoration of the parathyroid function and improve long-term outcomes. Why some parathyroid glands remain alive for months without secreting IPTH to then recover its functional properties remains a mystery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Powers J, Joy K, Ruscio A, et al. Prevalence and incidence of hypoparathyroidism in the United States using a large claims database. J Bone Miner Res 2013;28:2570-6. [Crossref] [PubMed]
- Edafe O, Antakia R, Laskar N, et al. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg 2014;101:307-20. [Crossref] [PubMed]
- Lorente-Poch L, Sancho JJ, Muñoz-Nova JL, et al. Defining the syndromes of parathyroid failure after total thyroidectomy. Gland Surg 2015;4:82-90. [PubMed]
- Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: Pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 2007;245:604-10. [Crossref] [PubMed]
- Carr AA, Yen TW, Fareau GG, et al. A single parathyroid hormone level obtained 4 hours after total thyroidectomy predicts the need for postoperative calcium supplementation. J Am Coll Surg 2014;219:757-64. [Crossref] [PubMed]
- Lorente-Poch L, Sancho JJ, Ruiz S, et al. Importance of in situ preservation of parathyroid glands during total thyroidectomy. Br J Surg 2015;102:359-67. [Crossref] [PubMed]
- Paloyan E, Lawrence AM, Paloyan D. Successful autotransplantation of the parathyroid glands during total thyroidectomy for carcinoma. Surg Gynecol Obstet 1977;145:364-8. [PubMed]
- Olson JA Jr, DeBenedetii MK, Baumann DS, et al. Parathyroid autotransplantation during thyroidectomy. Ann Surg 1996;223:472-8; discussion 478-80. [Crossref] [PubMed]
- Zedenius J, Wadstrom C, Delbridge L. Routine autotransplantation of at least one parathyroid gland during total thyroidectomy may reduce permanent hypoparathyroidism to zero. Aust N Z J Surg 1999;69:794-7. [Crossref] [PubMed]
- Promberger R, Ott J, Kober F, et al. Intra- and postoperative parathyroid hormone-kinetics do not advocate for autotransplantation of discolored parathyroid glands during thyroidectomy. Thyroid 2010;20:1371-5. [Crossref] [PubMed]
- Moley JF, Skinner M, Gillanders WE, et al. Management of the parathyroid glands during preventive thyroidectomy in patients with Multiple Endocrine Neoplasia Type 2. Ann Surg 2015;262:641-6. [Crossref] [PubMed]
- Prichard RS, Edhouse PJ, Sidhu SB, et al. Post-operative partial hypoparathyroidism: an under-recognized disorder. ANZ J Surg 2011;81:524-7. [Crossref] [PubMed]
- Tartaglia F, Blasi S, Giuliani A, et al. Parathyroid autotransplantation during total thyroidectomy. Results of a retrospective study. Int J Surg 2016;28 Suppl 1:S79-83. [Crossref] [PubMed]
- Lorente-Poch L, Sancho J, Muñoz JL, et al. Failure of fragmented parathyroid gland autotransplantation to prevent permanent hypoparathyroidism after total thyroidectomy. Langenbecks Arch Surg 2017;402:281-7. [Crossref] [PubMed]
- Applewhite MK, White MG, Xiong M, et al. Incidence, risk factors, and clinical outcomes of incidental parathyroidectomy during thyroid surgery Ann Surg Oncol 2016;23:4310-5. [Crossref] [PubMed]
- Sitges-Serra A, Gallego-Otaegui L, Suárez S, et al. Inadvertent parathyroidectomy during total thyroidectomy and central neck dissection for papillary thyroid carcinoma. Surgery 2017;161:712-9. [Crossref] [PubMed]
- Sasson AR, Pingpank JF Jr, Wetherington RW, et al. Incidental parathyroidectomy during thyroid surgery does not cause transient symptomatic hypocalcemia. Arch Otolaryngol Head Neck Surg 2001;127:304-8. [Crossref] [PubMed]
- Sakorafas GH, Stafyla V, Bramis C, et al. Incidental parathyroidectomy during thyroid surgery: an underappreciated complication of thyroidectomy. World J Surg 2005;29:1539-43. [Crossref] [PubMed]
- Lin DT, Patel SG, Shaha AR, et al. Incidence of inadvertent parathyroid removal during thyroidectomy. Laryngoscope 2002;112:608-11. [Crossref] [PubMed]
- Gourgiotis S, Moustafellos P, Dimopoulos N, et al. Inadvertent parathyroidectomy during thyroid surgery: the incidence of a complication of thyroidectomy. Langenbecks Arch Surg 2006;391:557-60. [Crossref] [PubMed]
- Song CM, Jung JH, Ji YB, et al. Relationship between hypoparathyroidism and the number of parathyroid glands preserved during thyroidectomy. World J Surg Oncol 2014;12:200-9. [Crossref] [PubMed]
- Cho JN, Park WS, Min SY. Predictors and risk factors of hypoparathyroidism after total thyroidectomy. Int J Surg 2016;34:47-52. [Crossref] [PubMed]
- Sitges-Serra A, Ruiz S, Girvent M, et al. Outcome of protracted hypoparathyroidism after total thyroidectomy. Br J Surg 2010;97:1687-95. [Crossref] [PubMed]
- Ji YB, Song CM, Sung ES, et al. Postoperative hypoparathyroidism and the viability of the parathyroid glands during thyroidectomy. Clin Exp Otorhinolaryngol 2017;10:265-71. [Crossref] [PubMed]
- Lang BH, Chan DT, Chow FC, et al. The association of discoiored parathyroid glands and hypoparathyroidism following total thyroidectomy. World J Surg 2016;40:1611-7. [Crossref] [PubMed]
- Vidal Fortuny J, Belfontali V, Sadowski SM, et al. Parathyroid gland angiography with indocyanine green fluorescence to predict parathyroid function after thyroid surgery. Br J Surg 2016;103:537-43. [Crossref] [PubMed]
- Lang BH, Chan DT, Chow FC. Visualizing fewer parathyroid glands may be associated with lower hypoparathyroidism following total thyroidectomy. Langenbecks Arch Surg 2016;401:231-8. [Crossref] [PubMed]
- Akerström G, Malmaeus J, Bergström R. Surgical anatomy of human parathyroid glands. Surgery 1984;95:14-21. [PubMed]
- El Khatib Z, Lamblin J, Aubert S, et al. Is thymectomy worthwhile in central lymph node dissection for differentiated thyroid cancer? World J Surg 2010;34:1181-6. [Crossref] [PubMed]
- Pattou F, Combemale F, Fabre S, et al. Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg 1998;22:718-24. [Crossref] [PubMed]
- McCann LM, Beto J. Roles of calcium-sensing receptor and vitamina D receptor in the pathophysiology of secondary hyperparathyroidism. J Ren Nutr 2010;20:141-50. [Crossref] [PubMed]
- Brown EM. Four-parameter model of the sigmoidal relationship between parathyroid hormone release and extracellular callcium concentration in normal and abnormal parathyroid tissue. J Clin Endocr Metab 1983;56:572-81. [Crossref] [PubMed]
- Ramírez JA, Goodman WG, Gornbein J, et al. Direct in vivo comparison of calcium-regulated parathyroid hormone secretion in normal volunteers and patients with secondary hyperparathyroidism. J Clin Endocr Metab 1993;76:1489-94. [PubMed]
- Carrillo-López N, Alvarez-Hernández D, González-Suárez I, et al. Simultaneous changes in the calcium-sensing receptor and the vitamin D receptor under the influence of calcium and calcitriol. Nephrol Dial Transplant 2008;23:3479-84. [Crossref] [PubMed]
- Schindler S, Mannstadt M, Urena P, et al. PTH secretion in patients with chronic renal failure assessed by a modified CiCa clamp method: effects of a 1-year calcitriol therapy. Clin Nephrol 2004;61:253-60. [Crossref] [PubMed]
- Malberti F, Farina M, Imbasciati E. The PTH-calcium curve and set point of calcium in primary and secondary hyperparathyroidism. Nephrol Dial Transplant 1999;14:2398-406. [Crossref] [PubMed]
- Daher R, Lifante JC, Voirin N, et al. Is it possible to limit the risks of thyroid surgery? Ann Endocrinol (Paris) 2015;76:1S16-26.
- Seo ST, Chang JW, Jin J, et al. Transient and permanent hypocalcemia after total thyroidectomy: Early predictive factors and long-term follow-up results. Surgery 2015;158:1492-9. [Crossref] [PubMed]
- De Pasquale L, Sartori PV, Vicentini L, et al. Necessity of therapy for post-thyroidectomy hypocalcaemia: a multi-centre experience. Langenbecks Arch Surg 2015;400:319-24. [Crossref] [PubMed]
- Park I, Rhu J, Woo JW, et al. Preserving parathyroid gland vasculature to reduce post-thyroidectomy hypocalcemia. World J Surg 2016;40:1382-9. [Crossref] [PubMed]



