Predictive features associated with thyrotoxic storm and management
Introduction
Thyroid storm (TS) is an endocrine emergency characterized by a rapid systemic deterioration, with a high mortality rate over 10% of hyperthyroid patients (1); therefore, a rapid diagnosis and emergent treatment prevents a catastrophic outcome (2,3). In a recent manuscript, the TS is estimated to be 0.2 persons/100,000 population/year, accounting for 0.22% of all thyrotoxic patients (3). Occurrence is main frequent into female gender with a ratio female:male of about 3:1 (3). Additionally, pregnancy and post-partum period are triggering factors to develop TS due to redefinition of autoimmunity state (4). Nowadays, thyroid surgery is the mainly endocrine procedures carried out in the world (5) and the hyperactivity of thyroid tissue after sub-total thyroidectomy is the primarily aetiology of perioperative TS. It can also occur during the intra-op period as a result of uncontrolled follicular cells secretion. Otherwise, the onset rate correlated to endocrine surgery is decreasing according to recent preoperative indications that create an euthyroid state before performing surgery (6). Therefore, an unsuitable preoperative management is related to a disastrous outcome during preoperative, intraoperative and postoperative periods. The classical features of TS such as abdominal pain, diarrhoea, nervousness and restlessness are masked during general anaesthesia and only hyperthermia and cardiovascular effects could be the life threatening signs (7). Several conditions could simulate an inappropriate thyroid function and differential diagnoses [anaphylactic reaction, malignant hyperthermia, brain insult, phaeochromocytoma, neuroleptic malignant syndrome or untreated hypertension (8)] could determine an inappropriate management delay. This review analyses predictive features associated with thyrotoxic storm highlighting recent literature to optimize the patient quality of care.
Predictive features
TS is due to triggering conditions associated to unknown thyroid pathology (usually untreated or uncontrolled Graves’ disease). More rarely other thyrotoxic disorders, such as destructive thyroiditis, toxic multinodular goiter, TSH-secreting pituitary adenoma, hCG-secreting hydatidiform mole or metastatic thyroid cancer, cause TS (9-12). Triggering conditions could be drugs such as amiodarone, sorafenib, ipilimumab and inappropriate hormone ingestion (13-15) or medical settings as surgery, radioiodine therapy and exposure to excess iodine in patients with hyperthyroidism (2,5,16,17). For these reasons, in all patients with know or unknown abnormal thyroid function submitted to surgical procedures is necessary to assess the compliance to the prescribed therapy and to optimize hormonal secretion, to settle the better endocrinal function at hospitalization. During preoperative period a complete physical exam, focusing on cardiovascular signs, could suggests a clinical suspicion for thyrotoxicosis permitting to prevent perioperative systemic organ failure related to inappropriate hormonal excretion. When TS occurs, its mortality is approximately 11% (3) due to multiple organ failure. Acute heart failure is the initial event, followed by respiratory failure, disseminated intravascular coagulation (DIC), gastrointestinal signs, neurological collapse and sepsis (3). To reduce mortality and to improve survival rate early suspicion, prompt diagnosis and intensive treatment on presentation of TS are essential (18).
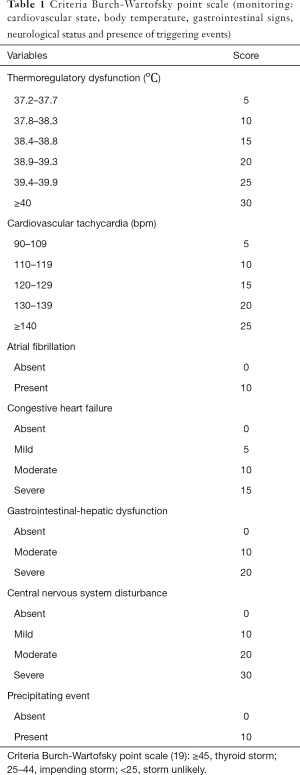
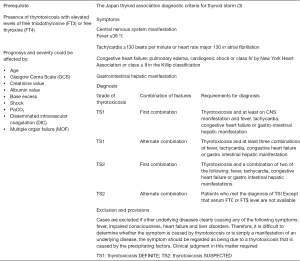
The Japan Thyroid Association and Japan Endocrine Society taskforce committee conducted nationwide surveys and developed new diagnostic criteria for TS, in addition to Burch and Wartofsky scale (3,19). The Burch-Wartofsky Point Scale (BWPS) for diagnosis of TS, proposed in 1993, is an empirically derived scoring system, which considers the precipitating factors and the severities of symptoms of multiple organ decompensation (thermoregulatory dysfunction, tachycardia/atrial fibrillation, disturbances of consciousness, congestive heart failure and gastro-hepatic dysfunction) (Table 1) (19). Instead, according to the Japanese Thyroid Association (JTA) diagnostic criteria, the presence of thyrotoxicosis is a prerequisite condition to confirm TS (Figure 1) (3). The 2016 guidelines for the management of TS in order to increase the accuracy of clinical diagnosis recommend use of both diagnostic systems to evaluate patients (18).
Full table
The presentation of TS includes fever, profuse sweating, signs of encephalopathy (anxiety, emotional lability, restlessness, agitation, confusion, delirium, frank psychosis, coma), various cardiac manifestations (sinus tachycardia, atrial arrhythmias, congestive heart failure), systolic hypertension, and gastrointestinal symptoms (diffuse abdominal pain with abnormal liver enzymes levels) (17). The major challenges of an intraoperative TS onset are due to several conditions that could mimic a cardiovascular collapse with thermoregulatory signs such as pain, electrolytes disturbances, malignant hyperthermia, heart failure and anaphylactic reactions (7).
Thyrotoxic storm management
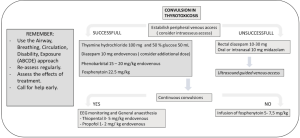
The pillar of TS management is to treat the hormonal excess excretion starting prematurely all supportive maneuvers. Admission into intensive care unit (ICU) is recommended for all patients, not only when heart failure, haemostatic disorders and multiple organ failure are occurred but also to optimize physiological conditions. The intraoperative approach recently published (18) appears the finest method to treat this disorder. After the confounding diagnostic criteria are excluded, the intraoperative treatment of haemodynamic instability includes use of antithyroid drugs (ATDs), inorganic iodide, β-blockers, antipyretics, steroids and vasoactive medication.
ATDs
Thionamides, propylthiouracil (PTU) and methimazole (MMI), are the mainstays to control the activity of increased thyroid hormone levels. The main action of ATDs is the direct inhibition of thyroid peroxidase in the thyroid gland, with reduction of synthesis of new hormone.
The American Thyroid Association (ATA) recommends the PTU, probably due to inhibition of type I deiodinase activity in the thyroid gland and in peripheral tissues (20). The Japan nationwide surveys shows there were no significant differences in mortality between TS patients treated with MMI or PTU (3).
However, ATDs should be administered as soon as possible when TS in Graves’ disease is diagnosed, but not in cases of TS by destructive thyroiditis, because ATDs are not effective against the destructive release of thyroid hormones stored in the gland and the recommended dose of PTU is 600 mg/die.
The MMI dose differ between oral intake and intravenous administration; it is 60 mg/day and 30 mg/die respectively.
Inorganic iodide
Inorganic iodide inhibiting iodide oxidation and organification (the Wolff-Chaikoff effect). It is widely used as pre-operatory treatment for thyroid surgery in order to decrease intraoperative bleeding, because inorganic iodide can reduce blood flow to the thyroid gland (21). Inorganic iodide should be administered simultaneously with ATDs in patients with TS with hyperthyroidism condition.
Corticosteroids
The hypermetabolic state related to TS could generate a depletion of stress hormones and corticosteroids should be administered as prophylaxis for related adrenal insufficiency.
Additionally, Bianco et al. (22) highlighted that large doses of corticosteroids inhibit thyroid hormone synthesis and peripheral conversion of T4 to T3. The recommended doses of corticosteroids are 300 mg/day hydrocortisone or 8 mg/day dexamethasone.
Antipyretics
The restoration of thermoregulation is mandatory to reduce all deleterious effects on coagulation, electrolytes balance and pH. Acetaminophen is the first choice and all mechanical refrigeration techniques such as cooling blankets or ice packs should be used in TS patients with resistant fever. Larsen et al. showed that salicylate could worsen the status increasing free thyroid hormone levels due to alterations of thyroxine binding proteins (23). Infections, with fever onset, could manifest TS (2) and a precocious antibiotic therapy has to be applied on patients with suspected thyroid disease before sepsis signs are evident (24).
Beta-adrenergic receptor antagonists (beta-AAS)
The treatment of hyperdynamic state related to inappropriate hormonal excretion is through beta-adrenergic receptor antagonist drugs. The principal drugs to treat supraventricular arrhythmias are endovenous landiolol and esmolol. The administration when heart rate is <80 bpm, systolic blood pressure <80 mmHg or cardiac index is ≤2.2 L/min/m2 is not indicated. In patients with severe pulmonary disease, such as asthma and COPD, verapamil or diltiazem are the better choice. The incidence of atrial fibrillation in TS is reported between 12% and 28% (25), with an increased mortality rate (3), probably due to an accelerated systemic hemodynamic deterioration status (18). When supraventricular tachycardia occurred with impaired hemodynamic status is necessary to proceed to cardioversion. Indeed, digitalis is useful in patients with normal renal function without hemodynamic failure.
TS can lead to acute congestive heart failure (CHF). In this case, invasive hemodynamic monitoring such as Swan-Ganz catheter is recommended for patients with symptoms and signs of pulmonary edema (Killip class ≥ III) (18,26). In this setting, respiratory management should include non-invasive positive pressure ventilation (NIPPV), or tracheal intubation according to neurologic, pulmonary and cardiac functional status. Administration of endovenous vasoactive drugs and diuretics should be considered in order to maintain cardiovascular tone, to reduce venous return. The use of extracorporeal supportive maneuvers is rare.
Additionally, neurologic manifestation is common (3); to treat disturbances of consciousness and psychosis the psychiatrist or neurologist consultation to select doses of psychotropic medications should be considered (17). When convulsions are present, benzodiazepines are first-line agents. Alternative drugs for resistant convulsions are fosphenytoin, phenobarbital and sodium thiopental (Figure 2) (27). Nowadays, the patients with central nervous manifestations and age major to 60 years have a higher mortality.
There is an increased risk of gastrointestinal haemorrhage, due to corticosteroids administration, coagulopathy and mechanical ventilation (3). Acid-suppressive drugs, such as proton pump inhibitors (PPIs) or histamine-2 receptor antagonists (H2As), are recommended (18).
Hepatic failure is not a rare complication. Actually, is recommended a carefully monitoring in patients with bilirubin levels >3.0 mg/dL. The emergency thyroidectomy could be the only solution to treat such complications and appropriate life support is suggested (19) including therapeutic plasmapheresis and haemodialysis (18).
Conclusions
The above-mentioned literature shows that TS is a life threating medical conditions due to excessive hormonal activity. Actually, TS is a dangerous expression of thyrotoxicosis precipitated by several events. The presence of heart collapse, coagulation abnormalities and organ failure determines a poor outcome and all the therapeutic strategies are involved to reduce hormonal activity, to prevent organ damage and to sustain vital capacity. All the supportive measures employed during preoperative, intraoperative and postoperative periods are directed to avoid complications. Therefore, a thyroid function investigation should be performed in every patient with abnormal findings, such as tachycardia, weight loss, and tremors. The physicians have not to delay all the necessary treatment when there is a clinical suspicion to increase quality care of TS patients, in order to improve the outcome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Palestini N, Valori MR, Carlin R, et al. Mortality, morbidity and long-term results in surgically treated hyperthyroid patients. Review of 597 cases. Acta Chir Scand 1985;151:509-13. [PubMed]
- Gavin LA. Thyroid crises. Med Clin North Am 1991;75:179-93. [Crossref] [PubMed]
- Akamizu T, Satoh T, Isozaki O, et al. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 2012;22:661-79. [Crossref] [PubMed]
- Waltman PA, Brewer JM, Lobert S. Thyroid storm during pregnancy. A medical emergency. Crit Care Nurse 2004;24:74-9. [PubMed]
- Dionigi G, Dionigi R, Bartalena L, et al. Current indications for thyroidectomy. Minerva Chir 2007;62:359-72. [PubMed]
- Kang YS, Kim JW, Hong KH. Thyroid storm during thyroidectomy of the thyrotoxicosis patient. Korean J Anesthesiol 1998;35:38590. [Crossref]
- Bajwa SJ, Sehgal V. Anesthesia and thyroid surgery: The never ending challenges. Indian J Endocrinol Metab 2013;17:228-34. [Crossref] [PubMed]
- Roizen MF. Anesthetic implications of concurrent diseases. Hyperthyroidism. In: Miller RD. Anesthesia, 6th edn. Philadelphia: Churchill Livingstone, 2000:928-9.
- Swinburne JL, Kreisman SH. A rare case of subacute thyroiditis causing thyroid storm. Thyroid 2007;17:73-6. [Crossref] [PubMed]
- Fujio S. Thyroid storm induced by TSH-secreting pituitary adenoma: a case report. Endocr J 2014;61:1131-6. [Crossref] [PubMed]
- Hwang W, Im D, Kim E. Persistant perioperative tachydardia and hypertention diagnosed as thyroid storm induced by a hydatidiform mole: a case report. Korean J Anesthesiol 2014;67:205-8. [Crossref] [PubMed]
- Naito Y, Sone T, Kataoka K, et al. Thyroid storm due to functioning metastatic thyroid carcinoma in a burn patient. Anesthesiology 1997;87:433-5. [Crossref] [PubMed]
- Georges JL, Normand JP, Leormand ME, et al. Life-threatening thyrotoxicosis induced by amiodarone in patients with benign heart disease. Eur Heart J 1992;13:129-32. [Crossref] [PubMed]
- Haraldsdottir S, Li Q, Villalona-Calero MA, et al. Case of sorafenib-induced thyroid storm. J Clin Oncol 2013;31:e262-4. [Crossref] [PubMed]
- Yu CY, Chopra IJ, Ha E. A novel melanoma therapy stirs up a storm: ipilimumab-induced thyrotoxicosis. Endocrinol Diabetes Metab Case Rep 2015;2015:140092. [PubMed]
- Tietgens ST, Leinung MC. Thyroid storm. Med Clin North Am 1995;79:169-84. [Crossref] [PubMed]
- Wartofsky L. Thyrotoxic storm. In: Braverman LE, Cooper DS. editors. Werner & Ingbar’s the Thyroid: A Fundamental and Clinical Text (10th). Philadelphia: Williams & Wilkins, 2012:481-6.
- Satoh T, Isozaki O, Suzuki A, et al. Guidelines for the management of thyroid storm from The Japan Thyroid Association and Japan Endocrine Society (First edition). Endocr J 2016;63:1025-64.
- Burch HB, Wartofsky L. Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am 1993;22:263-77. [PubMed]
- Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid 2016;26:1343-421. [Crossref] [PubMed]
- Ansaldo GL, Pretolesi F, Varaldo E, et al. Doppler evaluation of intrathyroid arterial resistances during preoperative treatment with Lugol’s iodide solution in patients with diffuse toxic goiter. J Am Coll Surg 2000;191:607-12. [Crossref] [PubMed]
- Bianco AC, Nunes MT, Hell NS, et al. The role of glucocorticoids in the stress-induced reduction of extrathyroidal 3,5,3’-triiodothyronine generation in rats. Endocrinology 1987;120:1033-8. [Crossref] [PubMed]
- Larsen PR. Salicylate-induced increases in free triiodothyronine in human serum: evidence of inhibition of triiodothyronine binding to thyroxin-binding globulin and thyroxin-binding prealbumin. J Clin Invest 1972;51:1125-34. [Crossref] [PubMed]
- Committee for sepsis registry, Japan Association of Intensive Medicine. Therapeutic Guideline for Sepsis 2012. Available online: http://www.jsicm.org/pdf/SepsisJapan2012.pdf
- Bar-Sela S, Ehrenfeld M, Eliakim M. Arterial embolism in thyrotoxicosis with atrial fibrillation. Arch Intern Med 1981;141:1191-2. [Crossref] [PubMed]
- JCS Joint Working Group. Guidelines for treatment of acute heart failure (JCS 2011). Circ J 2013;77:2157-201. [Crossref] [PubMed]
- Japanese Society of Neurology. The guideline for epilepsy treatment 2010. Available online: http://www.neurology-jp.org