Parathyroid hormone and serum calcium levels measurements as predictors of postoperative hypocalcemia in total thyroidectomy
Introduction
Hypocalcaemia frequently complicates patients who have undergone thyroid surgery, occurring in as many as 30% of patients (1).
Hypocalcemia is multifactorial and may be due primarily to parathyroid excision, devascularization, and gland impair, which may lead to transitory or permanent hypoparathyroidism (1-3). Accompanying process, for instance vitamin D insufficiency, calcitonin realizes, “hungry bone syndrome” definitely conduce to this state (2,4). Authors have analyzed simple, reliable and sensitive instruments that may predict postoperative hypocalcemia (2,5-10). Serial measures of parathyroid hormone (PTH) and blood serum-corrected calcium levels following surgery have since been verified and allowed for earlier supplementation with calcium and vitamin D (5-8). Furthermore, these predictors have also facilitated thyroid surgeons to carefully opt subjects who may warily undergo early discharge (11). Finally, hospital budget earnings have been accomplished (6,8).
In the current study, we evaluate the association between PTH level and postoperative hypocalcaemia among patients underwent total thyroidectomy.
Methods
This is an analytical study conducted on 40 total thyroidectomies at King Abdulaziz Medical City (National Guard Hospital), between July 2011 and July 2012. Formal approval by the hospital ethical commission was obtained for this audit.
We excluded subtotal thyroid excision, emithyroidectomies, completion thyroidectomy, central and extended lateral neck lymph node dissection, parathyroid gland surgery, abnormal serum albumin, abnormal pre-operative calcium, abnormal pre-operative PTH levels, renal insufficiency and pre-operative calcium replacement.
Sample size consisted of 32 women and 8 men, mean age of 45.1 years (range, 17 to 82 years ±14.7).
Serial blood exam testing protocol that included serum calcium and PTH was routinely applied at 6 hours following surgery.
Standard values for blood serum calcium ranged from 2.12 to 2.62 mmol/L (8.48–10.48 mg/dL).
Hypocalcemia was entitled with any of the following features: (I) adapted serum calcium of 1.90 mmol/L (7.6 mg/dL) or less; (II) signs and symptoms of hypocalcemia (i.e., peri-oral numbness, extremity digits paresthesia, positive Chovstek’s and/orTrousseau’s sign).
Statistical analysis
SPSS software and student’s t-test were utilized for testing the difference in the means of continuous variables. Non-Parametric Mann-Whitney test was applied in case of abnormally distributed data. Fischer exact test was used to test for the rate of hypocalcaemia between males and females.
The study was approved by Institutional Ethics Committee Board of King Abdulaziz Medical City (National Guard Hospital) (n. 2011/03) and written informed consent was obtained from all patients.
Results
As shown in Figure 1, following total thyroidectomy, 12.5% (4/32) women experienced transient hypocalcemia, on the contrary no men developed this morbidity. However, most probably due to small sample size, this difference was not statistically significant.

Mean postoperative serum calcium equable as follows: 2.26±0.11 mmol/L in men and 2.20±0.12 mmol/L in female while the mean PTH levels were as follows: 42.6±26.5 ng/L in men and 39.2±41.7 ng/L in female. The variance was non-significant (Table 1).
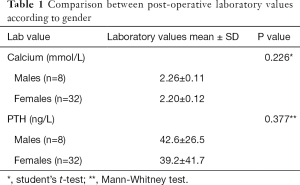
Full table
Erroneous presence of parathyroid gland in final histopathology specimen was associated with slightly but not significant lower mean serum calcium level (2.16±0.9 versus 2.22±0.12 mmol/L) (Table 2).
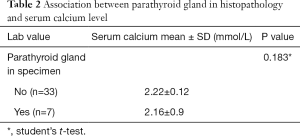
Full table
PTH level was significantly associated with post-thyroidectomy hypocalcaemia (43.7±39.3 versus 13.40±24.9 ng/L), P=0.014 (Table 3).
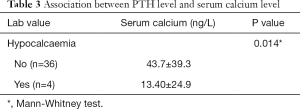
Full table
There is a positive concordance midmost the serum calcium and PTH levels postoperatively (r=0.42. P=0.007).
Minor asymmetry in gland volume and dominant nodule size were found between genders. Furthermore, negligible differences in the length of hospital stay were observed with and without post-thyroidectomy hypocalcaemia.
Discussion
There has been a considerable effort in recent years in identifying simple, reliable and sensitive tools that may anticipate the risk for postoperative hypocalcemia (2,3,5,7,9-12).
Sands et al., 2011 reported a higher percentage of post-thyroidectomy hypocalcemia within female (13). We failed to confirm such fact most probably due to relatively small sample size of the current survey. Although Sands’ analysis indicate that gender divergence is an distinct risk factor for developing hypocalcemia, the specific apparatus can only be assumed and may be associated to the effects of peculiar femininity steroids on the PTH metabolism.
Several researches have been realized on the utility of PTH to foresee hypocalcemia after total thyroidectomy using hemi-thyroidectomy procedure as control group (14-16). Grodski and Serpell evaluated 24 studies where the blood serum calcium determinations were tested as an internal dominate (17). There was critical disparity in study protocol among all papers considered by the Authors (17). Quick PTH was adopt in most studies and standard PTH was apply in other group. The timing of hormone sampling differs from trial to trial: in some analysis the sample was extract directly after thyroid gland excision and the authors tempt to use this early information to decide for parathyroid auto transplantation. Authors concluded that when a 75–80% PTH decline is experienced, auto transplant is advised. Other protocols used serial measurement taken just after skin closure, at 5, 10, 20 min to 1, 2, 4, up to 24 and 48 h.
Heterogeneity was found also in the method the experiments were computed. Some Authors identified an absolute cut-off PTH level to separate cases into normocalcemia and hypocalcemia subjects. Rather, others validated the percentage of PTH decline to predict this morbidity.
Most studies limited the evaluation to patients undergoing total or completion thyroidectomy. Some series included patients undergoing subtotal gland resection and hemithyroidectomy.
With regard to indication for surgery, most Authors except Graves’ disease and concurrent central neck dissection (CND) for cancer.
Despite above mentioned differences, there is a general agreement of conclusions with a robust affinity of postoperative PTH with post-thyroidectomy hypocalcemia development. Our study, although included relatively small size, confirmed the aforementioned finding.
Notwithstanding we can’t characterize an absolute PTH serum level or percentage hormone descend with 100% sensitivity and 100% specificity values.
Payne et al. tested PTH levels at 6, 12, and 20 h after their surgery: merging PTH and serum calcium measurement at 6 h would fairly establish subjects not at risk for hypocalcemia (18-22). Such arrangement was 100% specific, identified 68% of normocalcemic patients enduring for secure early discharge, determining a reduced hospital stay and budget. Lombardi et al. similarly found that PTH at 4–6 h to be a precise predictor of hypocalcemia (23,24).
Other Authors, nonetheless, suggested discontinuing the use of postoperative PTH for predicting hypocalcemia. Ghaheri et al. tested PTH just after thyroid procedure and discovered that low PTH levels corresponded with postoperative hypocalcemia but could not anticipate it. In this study of 500 consecutive total thyroidectomies, 38% developed hypocalcemia, found normal PTH levels 4 h postoperative in 70 hypocalcemic patients, 11 of whom were symptomatic (22). The Authors posted that PTH alone couldn’t precisely anticipate clinically relevant postoperative hypocalcemia.
Del Rio et al. reviewed 1,000 total thyroidectomies and analyzed the accuracy of a 24-h PTH measurement in predicting hypocalcemia (25). Two hundred and fifty-three subjects presented with hypocalcemia of which 152 evidenced at 24 h. 101 patients evolved in late (>24 h postoperative) hypocalcemia, 49 of these had low PTH levels at 24 h. Del Rio et al. assured that PTH determination at 24 h may not be prognostic (25).
In summary, PTH absolute levels and percentage decline test properly anticipate the risk of hypocalcemia although lack of 100% accuracy. Grave hypocalcemia is improbable in the context of a regular PTH level. Accordingly, PTH can be tested discreetly to expedite early and safe discharge. PTH levels can be used to assign prime calcium and/or vitamin D supplements treatment to prevent the frequency and grade of hypocalcemia morbidity.
Acknowledgements
Deep appreciation to Prof. Dionigi for his support, corrections, guidance and manuscript revision.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Glinoer D, Andry G, Chantrain G, et al. Clinical aspects of early and late hypocalcaemia afterthyroid surgery. Eur J Surg Oncol 2000;26:571-7. [Crossref] [PubMed]
- McHenry CR, Speroff T, Wentworth D, et al. Risk factors for postthyroidectomy hypocalcemia. Surgery 1994;116:641-7; discussion 647-8. [PubMed]
- Wingert DJ, Friesen S, Iliopoulos J, et al. Post-thyroidectomy hypocalcemia. Incidence and risk factors. Am J Surg 1986;152:606-10. [Crossref] [PubMed]
- Watson CG, Steed DL, Robinson AG, et al. The role of calcitonin and parathyroid hormone in the pathogenesis of post-thyroidectomy hypocalcemia. Metabolism 1981;30:588-9. [Crossref] [PubMed]
- Payne RJ, Hier MP, Tamilia M, et al. Postoperative parathyroid hormone level as a predictor of post-thyroidectomy hypocalcemia. J Otolaryngol 2003;32:362-7. [Crossref] [PubMed]
- Payne RJ, Tewfik MA, Hier MP, et al. Benefits resulting from 1- and 6-hour parathyroid hormone and calcium levels after thyroidectomy. Otolaryngol Head Neck Surg 2005;133:386-90. [Crossref] [PubMed]
- Payne RJ, Hier MP, Côté V, et al. Postoperative Parathyroid Hormone Levels in Conjunction with Corrected Calcium Values as a Predictor of Post-Thyroidectomy Hypocalcemia: Review of Outcomes 1 Year after the Implementation of a New Protocol. J Otolaryngol 2005;34:323-7. [Crossref] [PubMed]
- Payne RJ, Hier MP, Tamilia M, et al. Same-day discharge after total thyroidectomy: the value of 6-hour serum parathyroid hormone and calcium levels. Head Neck 2005;27:1-7. [Crossref] [PubMed]
- Lindblom P, Westerdahl J, Bergenfelz A. Low parathyroid hormone levels after thyroid surgery: a feasible predictor of hypocalcemia. Surgery 2002;131:515-20. [Crossref] [PubMed]
- Warren FM, Andersen PE, Wax MK, et al. Intraoperative parathyroid hormone levels in thyroid and parathyroid surgery. Laryngoscope 2002;112:1866-70. [Crossref] [PubMed]
- Chia SH, Weisman RA, Tieu D, et al. Prospective study of perioperative factors predicting hypocalcemia after thyroid and parathyroid surgery. Arch Otolaryngol Head Neck Surg 2006;132:41-5. [Crossref] [PubMed]
- Bourrel C, Uzzan B, Tison P, et al. Transient hypocalcemia afterthyroidectomy. Ann Otol Rhinol Laryngol 1993;102:496-501. [Crossref] [PubMed]
- Sands NB, Payne RJ, Côté V, et al. Female gender as a risk factor for transient post-thyroidectomy hypocalcemia. Otolaryngol Head Neck Surg 2011;145:561-4. [Crossref] [PubMed]
- Alía P, Moreno P, Rigo R, et al. Postresection parathyroid hormone and parathyroid hormone decline accurately predict hypocalcemia after thyroidectomy. Am J Clin Pathol 2007;127:592-7. [Crossref] [PubMed]
- Di Fabio F, Casella C, Bugari G, et al. Identification of patients at low risk for thyroidectomy-related hypocalcemia by intraoperative quick PTH. World J Surg 2006;30:1428-33. [Crossref] [PubMed]
- Lo CY, Luk JM, Tam SC. Applicability of intraoperative parathyroid hormone assay during thyroidectomy. Ann Surg 2002;236:564-9. [Crossref] [PubMed]
- Grodski S, Serpell J. Evidence for the role of perioperative PTH measurement after total thyroidectomy as a predictor of hypocalcemia. World J Surg 2008;32:1367-73. [Crossref] [PubMed]
- Payne RJ, Hier MP, Tamilia M, et al. Postoperative parathyroid hormone level as a predictor of post-thyroidectomy hypocalcemia. J Otolaryngol 2003;32:362-7. [Crossref] [PubMed]
- Payne RJ, Hier MP, Tamilia M, et al. Same-day discharge after total thyroidectomy: the value of 6-hour serum parathyroid hormone and calcium levels. Head Neck 2005;27:1-7. [Crossref] [PubMed]
- Payne RJ, Hier MP, Côté V, et al. Postoperative parathyroid hormone levels in conjunction with corrected calcium values as a predictor of post-thyroidectomy hypocalcemia: review of outcomes 1 year after the implementation of a new protocol. J Otolaryngol 2005;34:323-7. [Crossref] [PubMed]
- Payne RJ, Tewfik MA, Hier MP, et al. Benefits resulting from 1- and 6-hour parathyroid hormone and calcium levels after thyroidectomy. Otolaryngol Head Neck Surg 2005;133:386-90. [Crossref] [PubMed]
- Ghaheri BA, Liebler SL, Andersen PE, et al. Perioperative parathyroid hormone levels in thyroid surgery. Laryngoscope 2006;116:518-21. [Crossref] [PubMed]
- Lombardi CP, Raffaelli M, Princi P, et al. Parathyroid hormone levels 4 hours after surgery do not accurately predictpost-thyroidectomy hypocalcemia. Surgery 2006;140:1016-23. [Crossref] [PubMed]
- Lombardi CP, Raffaelli M, Princi P, et al. Early prediction of postthyroidectomy hypocalcemia by one single iPTH measurement. Surgery 2004;136:1236-41. [Crossref] [PubMed]
- Del Rio P, Arcuri MF, Ferreri G, et al. The utility of serum PTH assessment 24 hours after total thyroidectomy. Otolaryngol Head Neck Surg 2005;132:584-6. [Crossref] [PubMed]


