Siliconoma of the breasts
Introduction
Foreign material injection was a popular technique of aesthetic breast augmentation in many countries. Liquid silicone, oil, paraffin, polyacrylamide hydrogels, and unidentified liquid gels were injected into breast parenchyma (1). Nowadays, it is condemned by the legitimate plastic and reconstructive societies (2). However, a certain number of cases who have foreign material injection to their breasts still develop late sequelae and loco regional complications. The frequent late sequelae are infection, inflammation, silicone migration, disfiguration and painful breast lump. The injected material can migrate through lymphatic channel, ductal system or direct invasion.
The clinical presentations may mimic to breast cancer especially when associate with axillary or intramammary lymph node enlargement (2). Magnetic Resonance Imaging (MRI) is usually recommended in addition to mammogram and ultrasonogram to evaluate extension of the lesion and confirm oncologic assessment (3). Surgical removal of affected tissue is commonly mandatory for therapeutic purpose. Total mastectomy with or without preservation of skin/nipple areolar complex is an appropriate option for severely damage breast. Either immediate or delayed breast reconstruction should be considered as part of the treatment plan because these patients are likely to be young and concern of their aesthetic appearance. Autologous tissue is preferred over tissue expander prosthesis based reconstruction when presence of inflammation, infection or subcutaneous foreign material migration (1,4-6).
Limited number of literatures reported the successful tissue expander prosthesis based reconstruction after severe sequalae from post foreign material injection. We report our experience on tissue expander prosthesis based reconstruction after mastectomy for inflamed breast siliconoma.
Case report
Clinical presentation (Figure 1)
A 31 years old Thai woman presented with bilateral breast pain without fever. She had injection of liquid foreign material for breast augmentation and body sculpturing 3 years ago by non certified medical personnel. On physical examination, there were multiple painful breast lumps varying in size spread throughout both of her breasts. The overlying skin and subcutaneous layer was found indurated and stiffness with redness on the adjacent skin and nipple areola complexes. There was asymmetry of nipple areola complex level and symmastia with indurated tissue at lower sternal area. Two centimeters left axillary lymphadenopathy was also detected.
Surgical technique and intraoperative findings (Figure 2)
She was scheduled for bilateral mastectomy with removal of damaged subcutaneous layer and skin. Despite trying to preserve the healthy skin and nipple areola complex, however, we failed to preserve them because they were infiltrated by liquid silicone and severe fibrosis. The lymph nodes at left axilla were also removed. Tissue expanders (700 cc) were inserted in subpectoral plane with intraoperative filled 70 cc (10% volume) in both breasts.
Treatment outcomes
There was no immediate complication. We started to inflate tissue expander on post operative day 7th then continued weekly inflation until reaching target volume 700 cc at 12th week (Figure 3). We waited three months to allow the optimal tissue expansion effect before definitive prosthesis substitution.
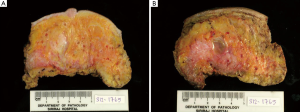
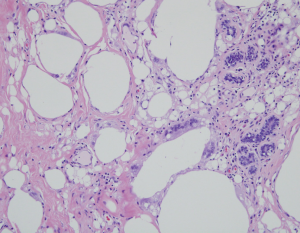
Pathological findings (Figure 4,5)
Both breasts from bilateral simple mastectomy displayed firm dull yellow grey white and breast tissue with scattered cysts varying from <0.1 to 0.5 cm in maximal diameter (Figure 4). The largest cyst, 1.5 cm in diameter containing clear oil-like material was seen in the left breast (Figure 4B). Foci of fibrosis and fat necrosis were seen. Microscopically, the breast lobules, fibrous and surrounding fatty tissue were infiltrated with macrophages and multinucleated foreign body type giant cells containing small and large clear vacuoles (Figure 5).
Discussion
The accurate incidence of foreign material injection for breast augmentation is difficult to study due to most of the procedures were performed illegally by non certified medical personnel. Most of the literatures are case reports or small case series. There is no available consensus or standardize guideline.
Most of the patients now usually present with late complications range from mild inflammation or small lump to severe mastitis or skin necrosis. The most important preoperative evaluation is to exclude the presence of incidental occult carcinoma. A study by Scaranelo and de Fatima Ribeiro Maia showed most frequent findings of mammogram and ultrasonogram were mammographic macronodular and mixed macronodular and micronodular patterns. Majority of ultrasonographic findings revealed the presence of marked echogenicity with snowstorm patterns. They concluded that both mammogram and ultrasonogram play role in identify free silicone in the breast tissue (7). However sensitivity of mammogram and ultrasonogram in detecting occult carcinoma is low. Peng et al. and Youk et al. successfully detected carcinomas in breasts injected with liquid silicone by MRI (3,8). A largest series by Luo et al. reported 235 patients with complications following Polyacrylamide hydrogel-injected breasts. They concluded that MRI is a sensitive and accurate method for diagnosis and treatment evaluation (9).
In general, neither liposuction nor curettage is sufficient enough to remove the granulomatous tissue. Surgical removal is mandatory and subcutaneous mastectomy is usually a recommendation (2,9). Many surgeons preferred autologous flap over the prosthesis for reconstructive option. Bilateral pedicled or free transverse rectus abdominis myocutaneous flap, deep inferior epigastric perforator flap are among the favorite choices (1,2,4-6). Luo et al., performed prosthesis reconstruction in 108 out of 235 patients who had mastectomy following Polyacrylamide hydrogel-injected breasts. They claimed that immediate or delayed prosthesis reconstruction can be an effective surgical treatment (9).
In asymptomatic case there is no consensus to perform prophylactic mastectomy. Even though there is a concern of developing carcinoma and late complications. The incidence of carcinoma has never been reported in a cohort study. We encourage skin/nipple sparing mastectomy as a surgical treatment of choice in case of no skin involvement. Immediate reconstruction should be carried out if there is no purulent infection. Two-stage reconstruction with tissue expander insertion followed by definitive implant substitution is an appropriate option. Although autologous flap reconstruction might be necessary when large amount of skin is removed, however tissue expander technique can be employed.
In the future, there should be a guideline for evaluation and treatment of this specific problem. The certain amount of patients will be likely to present with late complications. Moreover, the incidence of breast cancer increases with age, as a result, there will be a problem of cancer screening and cancer diagnosis. The association between cancer risk and granulomatous disease from foreign material intraparenchymal injection should be studied.
Conclusions
Late sequelae of foreign material breast injection are not uncommon. Not only painful granulomatous tissue and inflammatory reaction but also the association of carcinoma incidence and screening should be aware. Subcutaneous mastectomy with immediate two stage reconstruction with tissue expander insertion followed by definitive implant substitution is a safe option and can be an alternative procedure.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Chiu WK, Lee TP, Chen SY, et al. Bilateral breast reconstruction with a pedicled transverse rectus abdominis myocutaneous flap after subcutaneous mastectomy for symptomatic injected breasts. J Plast Surg Hand Surg 2012;46:242-7.
- Liu S, Lim AA. Evaluation and treatment of surgical management of silicone mastitis. J Cutan Aesthet Surg 2012;5:193-6.
- Peng HL, Wu CC, Choi WM, et al. Breast cancer detection using magnetic resonance imaging in breasts injected with liquid silicone. Plast Reconstr Surg 1999;104:2116-20.
- Aoki R, Mitsuhashi K, Hyakusoku H. Immediate reaugmentation of the breasts using bilaterally divided TRAM flaps after removing injected silicone gel and granulomas. Aesthetic Plast Surg 1997;21:276-9.
- Lai YL, Weng CJ, Noordhoff MS. Breast reconstruction with TRAM flap after subcutaneous mastectomy for injected material (siliconoma). Br J Plast Surg 2001;54:331-4.
- Ono S, Ogawa R, Takami Y, et al. A case of breast reconstruction with bilaterally divided transverse rectus abdominis musculocutaneous flaps after removal of injected silicone and granuloma. J Nippon Med Sch 2012;79:223-7.
- Scaranelo AM, de Fátima Ribeiro Maia M. Sonographic and mammographic findings of breast liquid silicone injection. J Clin Ultrasound 2006;34:273-7.
- Youk JH, Son EJ, Kim EK, et al. Diagnosis of breast cancer at dynamic MRI in patients with breast augmentation by paraffin or silicone injection. Clin Radiol 2009;64:1175-80.
- Luo SK, Chen GP, Sun ZS, et al. Our strategy in complication management of augmentation mammaplasty with polyacrylamide hydrogel injection in 235 patients. J Plast Reconstr Aesthet Surg 2011;64:731-7.





