Central round block repair of large breast resection defects: oncologic and aesthetic outcomes
Introduction
In contemporaneous practice 70% of women are suitable for wide local excision (WLE) followed by radiotherapy, which has been shown to be as effective as mastectomy in treating early breast cancer (1,2). Involved margins are a risk factor for local recurrence and acceptable rates of local recurrence for all breast cancer surgery are considered to be less than 3–5% at 5 years in the UK (3). Despite careful planning, up to 30% of WLEs lead to close or involved margins where further surgery for re-excision or mastectomy is then required (4-6). With continued improvement in patient survival following effective breast cancer treatment, patient expectation of good long-term cosmetic outcomes has also increased significantly.
Oncoplastic surgery has evolved as a hybrid of oncologic and plastic surgery techniques (7,8). Larger tumours can be excised with immediate repair allowing breast conservation in comparatively smaller breasts, potentially reducing margin involvement, whilst facilitating superior cosmetic outcomes. These techniques offer an alternative to mastectomy in patients that would have previously been denied breast conservation (9,10). A range of volume displacement techniques can be used to correct defects of up to 20% of breast tissue loss. Therapeutic reduction mammaplasty usually permit the greatest amount of volume displacement to correct large defects relative to breast size (7,8,11,12). Where resection requires less than 20% of the breast volume to be excised, skin excision is unlikely to be necessary (13). When the breast volume excised exceeds 20%, a formal mammoplasty incorporating skin excision is generally required (13).
The central round block repair is a volume displacement technique with varying amount of skin adjustment to take into account the volume loss or skin reduction requirement in breasts with low to moderate ptosis and hypertrophy. This modification of the circumareolar mammoplasty described by Benelli (14) has been adapted as an oncoplastic procedure (15-17). More recently, the technique has been applied in Asian women with smaller breast volumes in Japan (18), Korea (19) and Taiwan (20).
There are currently limited data on the likelihood of involved margins at primary resection, long-term oncological safety, aesthetic outcomes or the frequency of contralateral symmetrising surgery required following a round block repair of WLE defects. The aim of this study was to review a single institution’s experience of central round block repair and assess surgical, oncological and aesthetic outcomes.
Methods
A clinical audit with ethical committee approval (reference SAG30) of 57 consecutive patients in a single tertiary referral institution were included. All patients underwent a central round block repair of WLE defects over a 4-year period from January 2008 to January 2012. Patients with a median follow-up of 5 years (range, 1.9–8.4 years) were included. Patients were selected based on the size of the tumour in relation breast volume and position. All were advised that a simple resection and advancement/rotation glanduloplasty alone would have left a significant residual contour deformity with excess skin envelope laxity. Every woman would have been suitable for a therapeutic reduction mammoplasty but the aim was to perform a simpler procedure with less scarring and to reduce the need for symmetrising surgery. Patients were excluded if they chose to have a therapeutic reduction mammoplasty (n=12) or a mastectomy (n=4) instead of the suggested round block technique.
Patients who needed further surgery for close or involved margins either had further margin resection or completion mastectomy. Adjuvant therapy recommendations were based on the final surgical pathology. All complications and their treatment along with secondary procedures to either the ipsilateral or contralateral breast were recorded. Complete data on oncologic outcomes of local recurrence and overall survival were obtained by case note review of the institutional electronic patient record.
Operative technique (Figure 1)
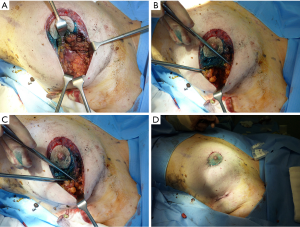
The required excision was planned preoperatively depending on the size and location of the tumour. A concentric circumareolar ring was marked and de-epithelialized to reduce the skin envelope sufficiently to account for both the reduction in volume as a result of the excision and any additional cosmetic benefit from a skin tightening mastopexy. A spherical block of tissue was removed from the subcutaneous fat down to the pectoral fascia with the intention of a 1 cm macroscopic margin. Excising this tissue as a radially orientated ellipse of parenchymal tissue may facilitate closure (Figure 1A). Any glandular dog-ears arising were excised under the skin flaps when closing if required.
For the repair, adjacent breast skin was widely undermined in the mastectomy plane between the subcutaneous fat and the breast parenchyma at the level of the superficial fascia. The parenchymal breast tissue was mobilised in the pre-pectoral plane (Figure 1B). As much as half of the breast may need to be undermined to facilitate sufficient mobilisation of the underlying glandular tissue and to facilitate re-draping of the tightened skin envelope. The 2-0 monocryl sutures were used to close the parenchymal defect radially and re-cone the breast tissue (Figure 1C). This can be used for all peripheral tumours. Central tumours may require a tri-radiant or “Mercedes-Benz” closure, excised initially as a cylinder and closed as appropriate. The skin was then re-draped accounting for contour irregularities. The dermis was closed with deep, buried, interrupted 2-0 vicryl-plus and a continuous subcuticular suture with 3-0 monocryl, reinforced by tissue glue and covered by water-resistant dressings (Figure 1D). Patients were treated as day cases and no drains were required.
Estimated volume of breast volume resected
Preoperative mammograms were reviewed and the estimated percentage of breast volume resected calculated using a method previously described by Katariya et al. (21) and validated previously in the assessment of cosmetic defects after breast conservation surgery by Cochrane et al. (22). In brief, the estimate assumes the tumour to be a sphere and the estimated macroscopic resection undertaken with a planned 1 cm margin. The formula used to calculate this from the MLO view was 4/3πr3. The breast volume was estimated to be a cone based on the formula 1/3πR2h. Resolving this equation gave an estimated percentage of breast volume excised of 4πr3/πR2h where r = tumour radius +1 cm, R = breast radius and h = breast projection.
Photographs
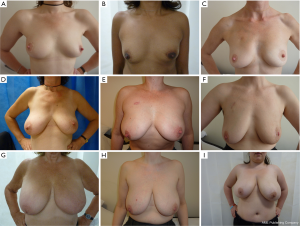
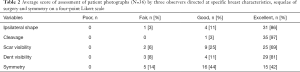
Three observers evaluated patients’ photographs, taken at their last follow-up appointment, in frontal views with arms in the neutral position on the hips (Figure 2), with arms raised and in profile. The three assessors were two surgeons (GP Gui and J Lee) and a specialist nurse practitioner (M Concepcion). Patients were assessed for shape, cleavage, scar visibility, volume deficit symmetry using a Likert scale scored for poor, fair, good and excellent. As there were three observers, the median score was used, thus accounting for any non-concordance between the three assessors for each parameter evaluated in individual patients
Measurements
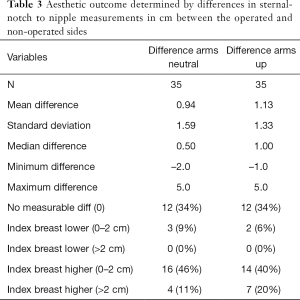
Sternal-notch-nipple distances with the hands on the hips were measured as an indicator of deviation of symmetry between the index and contralateral side in the neutral position. Sternal-notch-nipple distances were also measured with arms above the head. Measurements were taken pre-operatively and at their latest follow-up appointment. Both measurements were recorded and related to the site of tumour resection within the breast and the volume of excision as an indicator of factors that might influence symmetry after surgery.
Results
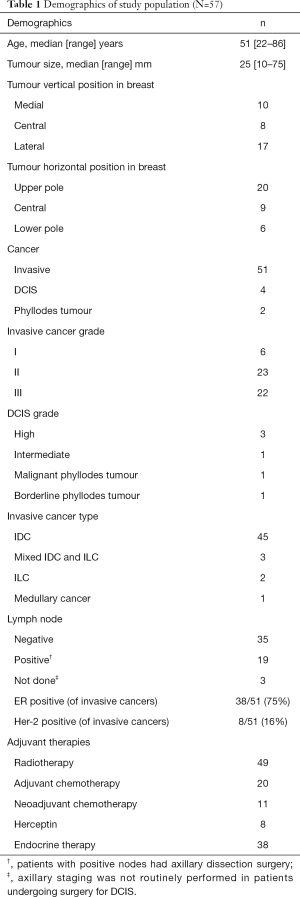
The median patient age at time of surgery was 51 (range, 22–86) years. The median follow-up duration was 5 (range, 1.9–8.4) years. The median specimen weight resected was 50 (range, 25–361) g and the median tumour size resected was 25 (range, 10–75) mm. The patient demographics and tumour profiles are summarized in Table 1. The median diameter of the estimated resection was 4.8 cm (range, 3.0–9.4 cm) and the median estimated percentage volume of breast excised using mammographic geometric estimation was 17.8% (range, 6–31%).
Full table
Three clinically significant seromas occurred. One was treated successfully by aspiration, one became infected that required intravenous antibiotics and the third developed an encapsulated seroma that was subsequently excised. Seven patients reported swelling attributed to a small seroma on ultrasound scan that could not be delineated clinically and was managed conservatively. All of these settled spontaneously with no further intervention. There were two other infections defined by mild erythema which required antibiotics and one patient had a small superficial wound dehiscence. All of these were managed conservatively. One patient had persistent pain in the breast at 2 years and one patient developed limited shoulder abduction requiring prolonged physiotherapy.
In total, 12/57 patients required further surgery for close margins clear by less than 2 mm (95% CI, 12–33). Five patients proceeded to successful wider re-excision and seven women had a completion mastectomy, usually for multiple involved margins.
There were two local recurrences in the follow-up period. One of these occurred in a patient who had declined the recommended adjuvant breast radiotherapy. Five patients developed distant metastases (one lung, one brain, one liver, one bone and one bone with brain), four of whom died from their disease. One patient died from other causes.
Aesthetic outcomes were evaluated in 50/57 patients after excluding the seven patients who required a mastectomy. No patient had clinically significant asymmetry pre-operatively. There was incomplete data for photographic assessment in 14 patients. The median of all three observers assessing photographic outcome is shown in Table 2. There was no statistical significant difference in symmetry between the location in the breast of tumour resection, with similar proportions of poor and good outcome assessed using Fisher’s exact test (data not shown).
Full table
Patients’ sternal notch-to-nipple distance were measured with the arms in the neutral position and with the arms above the head. Data were available from 35 patients and showed no significant differences in nipple height between the operated and non-operated sides. There was no measurable asymmetry in any parameter in 12 patients (34%). The 31/35 (88.6%) of patients had a final nipple position to match the unoperated contralateral side for symmetry within 2 cm (Table 3). In those where there was a measurable difference, only two elected to have surgery to the contralateral side for symmetry, with no patients planning or awaiting further secondary surgery at the time of census.
Full table
The sector of the breast involved was assessed as a factor contributing to measured differences in sternal notch to nipple distances. There was a small statistically significant difference in sternal notch-nipple distance if the tumour was located in the upper rather than the central/lower horizontal sectors of the breast which resulted in the nipple on the index side being slightly higher (P=0.038, Kruskal-Wallis test).
Discussion
A recent systematic review by Haloua et al. (23) identified 12 publications between 2000 and 2011 assessing oncoplastic breast surgery that fulfilled adequate criteria for analysis (19,24-34). No randomized controlled trials were identified. In these studies, 80% to 93% of patients had invasive tumors; cancer-free resection margins were observed in 78% to 93%, resulting in a 3% to 16% mastectomy rate. Local recurrence rates were 0% to 7%. Good cosmetic outcomes were achieved in 84% to 89% of patients. The authors commented that most studies showed significant weaknesses including lack of robust design and methodological shortcomings. Well-designed prospective longitudinal studies with adequate follow-up are the only realistic way in which critics, who remain unconvinced by the existing data over three decades of oncoplastic surgery may be silenced (35-39).
Breast conservation surgery is well established and the desire to achieve optimum aesthetic results is a natural continuation in the development of oncoplastic surgery. The predictable factors which increase the risk of local recurrence following breast conservation include age, tumour size, lymph node involvement, tumour histologic type, grade and hormone receptor status (6,40-42). The only parameter that can be influenced by surgery is the achievement of clear surgical margins. Incomplete or uncertain surgical margins were shown in a meta-analysis with rigorous methodology to have an odds ratio of 2.44 for local recurrence when compared to clear margins (6,43). Margin re-excision is often technically difficult to achieve with absolute certainty, particularly after the tissue rearrangement involved in some complex oncoplastic procedures. Some surgeons therefore elect to perform these procedures staged and reconstruct after histological confirmation of clear margins are obtained. The simplicity of the round block technique favours the ability to perform a re-excision of margins compared to wise pattern mammoplasty approaches. In our series, there were 5/12 patients with involved margins having a successful cavity re-excision. The circumareolar incision also allows easy incorporation of the pre-existing surgical scar into mastectomy planning should this be required to achieve adequate oncologic excision.
Definition of margins extend beyond surgical technique. Variables such as surgical orientation of the specimen and the methods used by pathologists to process tissue also make the reproducibility of pathological and oncological outcomes between different centres difficult. The agreement of what constitutes a clear margin also varies between units and remains an international area of controversy despite the recent ASCO guidelines (44). Whilst extensive DCIS is associated with local recurrence (45), clear excision margins after breast conservation are still considered adequate when followed with adjuvant radiotherapy. Modern adjuvant treatments have significantly helped to reduce local recurrence and the multimodal treatment required to treat breast cancer is established as gold standard. Future horizons are likely to see the development of better selection tools to identify patients for therapies that may extend beyond chemotherapy, radiotherapy and endocrine therapy, into an arena of personalized treatment strategies, and targeted immunotherapy.
Oncoplastic surgery represents an excellent alternative to mastectomy where the resection might otherwise have necessitated a more radical procedure with better aesthetic outcomes than would be possible with simple WLE. The messages from the current literature are clear: oncologically, patients should be appropriately selected for segmental resection to achieve complete excision, excluding patients with multicentric disease across different sectors of the breast where breast conservation is unlikely to be successful. Aesthetically, patients are selected based on tumour size in relation to the size of the breast, the position of the tumour, and the tissue elasticity (8,12). This study contributes to this further by showing that good aesthetic and oncological results can be obtained for tumours in all sectors of the breast, including central tumours.
This study represents a comprehensive prospective evaluation of oncologic parameters and complications in central round block repairs with circumareolar skin reduction in a cohort of patients with long term follow-up. The prospective data for this technique show good aesthetic outcomes can be achieved with reproducible results. The technique is oncologically safe with low complication and comparable local recurrence rates to breast conservation surgery in general or other oncoplastic techniques. Large proportional oncologic resection to breast size can be achieved and the technique is not limited to small breasts.
Low rates of planned and subsequent contralateral surgery can be expected with excellent measured symmetry at follow-up. Younger patients with good tissue elasticity may have an advantage to be exploited in this technique allowing better symmetry with the un-operated side without contralateral symmetrisation. It is prudent to limit the dissection in the pre-pectoral plane given the extent of subcutaneous undermining to ensure maximum vascularity to the glandular flaps. This may be particularly important in fatty breasts. However, our study shows that this technique gives safe and predictable results in patients of all ages regardless of the breast gland and fat composition. Clough et al. describes this point of principle with reference to choice of oncoplastic techniques in fatty/glandular breast types which we can validate for the central round block procedure in this study (13). We acknowledge that one criticism of the circumareolar round block mammoplasty is that it flattens the breast mound slightly. Although this was not specifically looked for in our series, it has not been a significant limitation noted by patients. Projectional differences such as this may also be difficult to demonstrate on conventional two dimensional photographs. Whilst any breast surgery involving circumareolar incisions can affect nipple sensation that may be worsened by radiotherapy, the authors believe these changes are less marked compared to therapeutic mammoplasties where surgical incisions are longer and greater volumes of breast tissue are resected.
A preferred outcome measure for breast aesthetics including reconstructive surgical procedures is now patient recorded outcomes (PROMS). Tools such as the BREASTQ have been developed relatively recently and provide excellent data on how patients feel about their surgery. We did not apply these current techniques to our historical and large cohort of patients with now mature data accumulated over several years. Future PROMS data with defined long-term outcomes would certainly be helpful in assessing the results of this, and indeed other, oncoplastic techniques.
The authors advocate the use of the central round block technique in patients of any age, with a wide range of breast size, shape and composition, various degrees of ptosis and all tumour positions within the breast to good effect. It is a simple procedure that gives good results with minimal compromise of future mastectomy and reconstructive options in the event of failed conservation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Royal Marsden Ethics Committee (No. SAG30) and written informed consent was obtained from all patients.
References
- Fisher B, Anderson S, Bryant J, et al. 20-year follow-up of a randomised trial comparing total mastectomy, lumpectomy and lumpectomy + irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233-41. [Crossref] [PubMed]
- Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227-32. [Crossref] [PubMed]
- Rainsbury D, Willett A. Oncoplastic Breast Reconstruction: Guidelines for Best Practice. BAPRAS/ABS Publication, 2012.
- Kaufmann M, Morrow M, von Minckwitz G, et al. Locoregional treatment of primary breast cancer: consensus recommendations from an International Expert Panel. Cancer 2010;116:1184-91. [Crossref] [PubMed]
- Park CC, Mitsumori M, Nixon A, et al. Outcome at 8 years after breast conserving surgery and radiation therapy for invasive breast cancer: influence of margin status and systemic therapy on local recurrence. J Clin Oncol 2000;18:1668-75. [Crossref] [PubMed]
- Singletary SE. Surgical margins in patients with early-stage breast cancer treated with breast conservation therapy. Am J Surg 2002;184:383-93. [Crossref] [PubMed]
- Clough KB, Nos C, Salmon RJ, et al. Conservative treatment of breast cancers by mammoplasty and irradiation: a new approach to lower quadrant tumours. Plast Reconstr Surg 1995;96:363-70. [Crossref] [PubMed]
- McCulley SJ, Macmillan RD. Planning and use of therapeutic mammoplasty--Nottingham approach. Br J Plast Surg 2005;58:889-901. [Crossref] [PubMed]
- Hamdi M. Oncoplastic and reconstructive surgery of the breast. Breast 2013;22:S100-5. [Crossref] [PubMed]
- Losken A, Dugal CS, Styblo TM, et al. A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plast Surg 2014;72:145-9. [Crossref] [PubMed]
- Kroll SS, Singletary SE. Repair of partial mastectomy defects. Clin Plast Surg 1998;25:303-10. [PubMed]
- Clough KB, Ihrai T, Oden S, et al. Oncoplastic surgery for breast cancer based on tumour location and a quadrant-per-quadrant atlas. Br J Surg 2012;99:1389-95. [Crossref] [PubMed]
- Clough KB, Kaufman GJ, Nos C, et al. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol 2010;17:1375-91. [Crossref] [PubMed]
- Benelli L. A new periareolar mammoplasty: the “round block” technique. Aesthetic Plast Surg 1990;14:93-100. [Crossref] [PubMed]
- Masetti R, Pirulli PG, Magno S, et al. Oncoplastic techniques in the conservative surgical treatment of breast cancer. Breast Cancer 2000;7:276-80. [Crossref] [PubMed]
- Amanti C, Moscaroli A, Lo Russo M, et al. Periareolar subcutaneous quadrantectomy: a new approach in breast cancer surgery. G Chir 2002;23:445-9. [PubMed]
- Giacalone PL, Dubon O, Roger P, et al. Doughnut mastopexy lumpectomy versus standard lumpectomy in breast cancer surgery: A prospective study. Eur J Surg Oncol 2007;33:301-6. [Crossref] [PubMed]
- Ogawa T. Usefulness of breast-conserving surgery using the round block technique or modified round block technique in Japanese females. Asian J Surg 2014;37:8-14. [Crossref] [PubMed]
- Yang JD, Bae SG, Chung HY, et al. The usefulness of oncoplastic volume displacement techniques in the superiorly located breast cancers for Korean patients with small to moderate-sized breasts. Ann Plast Surg 2011;67:474-80. [Crossref] [PubMed]
- Chen DR. An optimized technique for all quadrant oncoplasty in women with small- to medium-sized breasts. Eur Rev Med Pharmacol Sci 2014;18:1748-54. [PubMed]
- Katariya RN, Forrest AP, Gravelle IH. Breast volumes in cancer of the breast. Br J Cancer 1974;29:270-3. [Crossref] [PubMed]
- Cochrane RA, Valasiadou P, Wilson AR, et al. Cosmesis and satisfaction after breast-conserving surgery correlates with the percentage of breast volume excised. Br J Surg 2003;90:1505-9. [Crossref] [PubMed]
- Haloua MH, Krekel NM, Winters HA, et al. A Systematic Review of Oncoplastic Breast-Conserving Surgery. Current Weaknesses and Future Prospects. Ann Surg 2013;257:609-20. [Crossref] [PubMed]
- Bong J, Parker J, Clapper R, et al. Clinical series of oncoplastic mastopexy to optimize cosmesis of large-volume resections for breast conservation. Ann Surg Oncol 2010;17:3247-51. [Crossref] [PubMed]
- Chan SW, Cheung PS, Lam SH. Cosmetic outcome and percentage of breast volume excision in oncoplastic breast conserving surgery. World J Surg 2010;34:1447-52. [Crossref] [PubMed]
- Clough KB, Lewis JS, Couturaud B, et al. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg 2003;237:26-34. [Crossref] [PubMed]
- Giacalone PL, Roger P, Dubon O, et al. Comparative study of the accuracy of breast resection in oncoplastic surgery and quadrantectomy in breast cancer. Ann Surg Oncol 2007;14:605-14. [Crossref] [PubMed]
- Gulcelik MA, Dogan L, Camlibel M, et al. Early complications of a reduction mammoplasty technique in the treatment of macromastia with or without breast cancer. Clin Breast Cancer 2011;11:395-9. [Crossref] [PubMed]
- Kaur N, Petit JY, Rietjens M, et al. Comparative study of surgical margins in oncoplastic surgery and quadrantectomy in breast cancer. Ann Surg Oncol 2005;12:539-45. [Crossref] [PubMed]
- Meretoja TJ, Svarvar C, Jahkola TA. Outcome of oncoplastic breast surgery in 90 prospective patients. Am J Surg 2010;200:224-8. [Crossref] [PubMed]
- Rietjens M, Urban CA, Rey PC, et al. Long-term oncological results of breast conservative treatment with oncoplastic surgery. Breast 2007;16:387-95. [Crossref] [PubMed]
- Rusby JE, Paramanathan N, Laws SA, et al. Immediate latissimus dorsi miniflap volume replacement for partial mastectomy: use of intra-operative frozen sections to confirm negative margins. Am J Surg 2008;196:512-8. [Crossref] [PubMed]
- Veiga DF, Veiga-Filho J, Ribeiro LM, et al. Quality-of-life and self-esteem outcomes after oncoplastic breast-conserving surgery. Plast Reconstr Surg 2010;125:811-7. [Crossref] [PubMed]
- Veiga DF, Veiga-Filho J, Ribeiro LM, et al. Evaluations of aesthetic outcomes of oncoplastic surgery by surgeons of different gender and specialty: a prospective controlled study. Breast 2011;20:407-12. [Crossref] [PubMed]
- Kabir SA, Stallard S, Weiler-Mithoff E, et al. Six-year follow-up of patients treated with oncoplastic reduction mammoplasty: A cohort study. Int J Surg 2016;26:38-42. [Crossref] [PubMed]
- De Lorenzi F, Hubner G, Rotmensz N, et al. Oncological results of oncoplastic breast-conserving surgery: Long term follow-up of a large series at a single institution: A matched-cohort analysis. Eur J Surg Oncol 2016;42:71-7. [Crossref] [PubMed]
- Rezai M, Kraemer S, Kimmig R, et al. Breast conservative surgery and local recurrence. Breast 2015;24:S100-7. [Crossref] [PubMed]
- Semprini G, Cattin F, Vaienti L, et al. Oncoplastic surgery and cancer relapses: cosmetic and oncological results in 489 patients. Breast 2013;22:946-51. [Crossref] [PubMed]
- Chakravorty A, Shrestha AK, Sanmugalingam N, et al. How safe is oncoplastic breast conservation? Comparative analysis with standard breast conserving surgery. Eur J Surg Oncol 2012;38:395-8. [Crossref] [PubMed]
- Aalders KC, van Bommel AC, van Dalen T, et al. Contemporary risks of local and regional recurrence and contralateral breast cancer in patients treated for primary breast cancer. Eur J Cancer 2016;63:118-26. [Crossref] [PubMed]
- Akay CL, Meric-Bernstam F, Hunt KK, et al. Evaluation of the MD Anderson Prognostic Index for local-regional recurrence after breast conserving therapy in patients receiving neoadjuvant chemotherapy. Ann Surg Oncol 2012;19:901-7. [Crossref] [PubMed]
- Pendlebury SC, Ivanov O, Renwick S, et al. Long-term review of a breast conservation series and patterns of care over 18 years. ANZ J Surg 2003;73:577-83. [Crossref] [PubMed]
- Houssami N, Macaskill P, Marinovich ML, et al. The association of surgical margins and local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy: a meta-analysis. Ann Surg Oncol 2014;21:717-30. [Crossref] [PubMed]
- Buchholz TA, Somerfield MR, Griggs JJ, et al. Margins for breast-conserving surgery with whole-breast irradiation in stage I and II invasive breast cancer: American Society of Clinical Oncology endorsement of the Society of Surgical Oncology/American Society for Radiation Oncology consensus guideline. J Clin Oncol 2014;32:1502-6. [Crossref] [PubMed]
- Vicini FA, Recht A, Abner A, et al. Recurrence in the breast following conservative surgery and radiation therapy for early-stage breast cancer. J Natl Cancer Inst Monogr 1992;11:33-9. [PubMed]


