Transoral thyroidectomy: why is it needed?
Endoscopic thyroidectomy has been carefully investigated since 2008 with a natural orifice transluminal endoscopic surgery (NOTES) throughout a sublingual, or via a trans-tracheal approach in order to perfect cosmesis, which is an entire scarless benefit in the skin (1-4).
The sublingual and the trans-tracheal approaches, originally performed in Germany, were discontinued after experimental and few clinical studies because of tissue bruise, organ damage, complications, laryngeal nerve injuries, restrictive surgical view and safeness, conversion, unavailability of instrumentation and difficulties due to limitation of instrumentation movement (1-5).
Table 1 constitutes a summary of the advantages and disadvantages of the transoral gland removal via the sublingual approach (1-4).
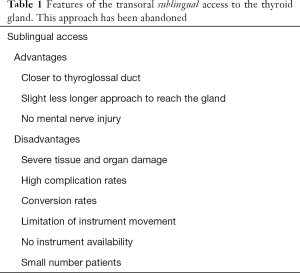
Full table
In 2013 a new NOTES procedure with an inferior 3-incision vestibular approach has been popularized for thyroid gland surgery in Thailand (5).
Prominent characteristics of transoral thyroidectomy (TOT) via three vestibular approaches are summarized in Table 2 and here below detailed presented.

Full table
Cosmesis
The main benefit and indication for TOT is the cosmetic result. Given the preeminence of thyroid surgery in young female patients, consideration should be given to reduce to the smallest as possible the invasiveness of the surgical procedure, secrete scars, that is improve cosmesis and the appearance of Patient after surgery (5). Cosmetics concerns, discussions and request, debated are a matter of some uncertainly, difficulty and frequently demanded from young woman and man and their partners, husbands, in the day life activity and work (5,6). Conventional thyroidectomy surgery include a transverse cervical incision, at least 3 cm long, that determine an appreciable mark left by healed wound (5). TOT in comparison to both conventional and other endoscopic thyroidectomy has the advantage of no visible incision in the skin, in the neck, and/or in other areas of the patient body (5-7). The three surgical incisions are weaved in the vestibular, lower lip. As a consequence, no physical or physiological complication related to scar as keloid, hypertrophic scar, contracture formation, dehiscence (8-10) (Figure 1).

Thus, the main usefulness of TOT is the extraordinary cosmetic result with no scar and possible emotional benefit and reassure (11,12).
Extensive inclusion criteria
TOT convoy a strict, precise yet wide inclusion criteria, i.e., (I) a preoperative ultrasonographically (US) estimated gland size <10 cm; (II) thyroid volume ≤45 mL; (III) dominant nodule size ≤50 mm; (IV) a benign lesions, like thyroid cyst, single-nodular goiter, or multinodular goiter; (V) Bethesda 3 or 4 lesion; (VI) papillary microcarcinoma without any evidence of metastasis (5-16).
The inclusion criteria are certainly broader than the other endoscopic or robotic procedures (5).
Exclusion criteria comprise patients who (I) are unfit for surgery; (II) cannot tolerate general anesthesia; (III) had antecedent radiation in the area of the head, neck and/or upper mediastinum; (IV) had previous neck surgery; (V) recurrent or huge goitre; (VI) thyroid gland volume >45 mL; (VII) dominant nodule size >50 mm; (VIII) evidence of lymph node or distant metastases; (IX) tracheal/esophageal invasion; (X) preoperative recurrent laryngeal nerve palsy (m) biochemical or US signs of hyperthyroidism and (XI) oral abscesses (5-16) (Table 3).
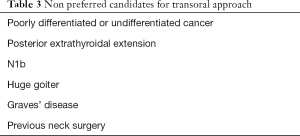
Full table
Minimally invasive procedure
In thyroid surgery, a minimally invasive surgery may be delineated by the length, site and total number of wounds, by the extent needed for careful and shortened dissection to extend in operation to the cervical area, the neck, the thyroid and parathyroid glands and the central compartment, reducing to the smallest as possible amount the tissue and organ trauma, maintaining safe visualization and exposure of the laryngeal nerves, the use or not of a videoscope and CO2 insufflation, enhancing cosmesis, the use of regional anesthesia, a painless procedure, duration of thyroidectomy or by an outpatient care setting (5-16).
The appellation of “minimal access” and “minimally invasive” are definitely not coincident in endocrine surgery (5-7). The MIVAT procedure is a minimally invasive because the surgical access is direct in the neck, with smaller extent of dissection and good cosmesis (9,12). Remote extracervical endoscopic thyroidectomies as the bilateral axillary breast approach (BABA) or the axilla approaches maybe not minimally invasive as the area of surgical division is considerable (ports are far away from thyroid and this require a significant degree of operation) (5,13). MIVAT and extracervical thyroidectomies present discrete advantages, although none of them completely avoids a cutaneous scar in the neck, chest, breast or axilla area (6,7,10-16).
TOT is a minimally invasive procedure as its vestibular access is near to the thyroid gland, the length of dissection guarantee less operation (5). The route, the way, the approach to the anterior neck is close, shorter than that from the axilla, or breast, or retroauricular (13-16). The transoral approach respects surgical anatomical subplatysmal planes (5). The flap dissection is similar to that of conventional surgery (16).
TOT preserve bilateral gland exploration
TOT is through a central-median approach, thus it provides the required secure bilateral view and exposure of thyroid gland and the two-sided procedure can be perform in safety without additional incisions (16).
Differently other endoscopic and robotic-assisted approaches that have a lateral remote access (as in the axilla, or retroauricular), TOT approach provides a midline access and main laid line exposure to the isthmus, both the right and left thyroid lobes in their completeness (superior and inferior pole, posterior gland), pyramidal lobe, the two inferior laryngeal nerves and superior laryngeal nerves, parathyroid glands and the lymph nodes in the central compartments, level 6 around the RLNs, trachea and esophagus (7,9). Central compartment inspection, dissection with complete lymphadenectomy was described and is feasible and safe (5-16).
TOT represents an appreciable opportunity over the other remote techniques (transaxillary BABA), in which approaching the contralateral thyroid lobe, central compartment lymph nodes and pyramidal lobe is actually demanding even for the experienced surgeon (12).
The sight from the 30° HD endoscope during the transoral approach, is cranial to caudal, and this is a well-acquainted frame for the surgeon routinely involved in conventional thyroid surgery for identifying the laryngeal nerves, parathyroids glands and provides excellent exposure, allowing a complete central neck dissection (12,13).
Feasible with both conventional endoscopic and robot instrumentation
Robotic surgery is now well established in neck thyroid surgery with significant advantages, as for the more precise dissection, no tremor, perfect vision quality with 3D HD monitors, curved instruments, less collision with arms, counter traction by the additional 4th axilla port and larger specimens removal.
However, Robot is not yet executed widely because of obstacles in the economy (5). The robotic technology is at the present time accessible for a confined number of Hospitals especially in the USA, Asian Countries as the Republic of Korea, few European Institutions (5).
The rating use of routine conventional laparoscopic endoscopic instrumentation for TOT seems to be a more feasible option for wide adaption of this new technique (6). TOT can be carried with or without the aid of the robot, and safely with only the use of conventional endoscopic instruments (Figure 2). De facto, TOT is done fully endoscopically using conventional endoscopic instruments with less overall operative time (14).
Reproducibility
TOT is currently multi-institutional, internationally performed in Asia, Europe, Latin America and USA. TOT is being embraced by several high volume experienced centers as in Thailand (40 centers), South Korea (3 centers, robotically), India, China (2 centers), Singapore, Taiwan (20 centers), USA (7 centers), Mexico, Japan, Ecuador and Italy (16).
Surgeons now performing TOT are expertise with profound background of endocrine diseases, conventional thyroidectomy, endoscopically and robotic procedures, this is a prerequisite for a safe introduction of TOT (5).
Reliable postoperative course
Postoperative course of TOT is reliable and steady (Table 4). For TOT, no dressing is required. No skin wound care is necessary. Oral antibiotics and mouthwash 3 times per day are prescribed for 3–5 days (5). Patients are mobilized from bad at +4 hrs postoperatively (5). Most patients start an oral soft diet on day 0 on same evening of surgery (5). Patients can have a shower in the evening and men can shave. Patients can sunbathe on the following weekend (5). Discharge from hospital are dictated by the common rules of the thyroid surgery, after careful evaluation by the surgeon, endocrinological and anesthesiological specialist, serum calcium dosage and after neck, mouth, vestibule and laryngoscopy to evaluate the RLNs function (5).
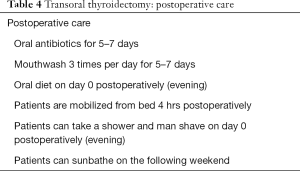
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. [Crossref] [PubMed]
- Benhidjeb T, Wilhelm T, Harlaar J, et al. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc 2009;23:1119-20. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Video. Endoscopic minimally invasive thyroidectomy: first clinical experience. Surg Endosc 2010;24:1757-8. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Liu E, Qadir Khan A, Niu J, et al. Natural Orifice Total Transtracheal Endoscopic Thyroidectomy Surgery: First Reported Experiment. J Laparoendosc Adv Surg Tech A 2015;25:586-91. [Crossref] [PubMed]
- Woo SH. Endoscope-assisted transoral thyroidectomy using a frenotomy incision. J Laparoendosc Adv Surg Tech A 2014;24:345-9. [Crossref] [PubMed]
- Benhidjeb T, Stark M. Endoscopic minimally invasive thyroidectomy (eMIT): safety first! World J Surg 2011;35:1936-7; author reply 1938-9.
- Clark JH, Kim HY, Richmon JD. Transoral robotic thyroid surgery. Gland Surg 2015;4:429-34. [PubMed]
- Lee HY, Richmon JD, Walvekar RR, et al. Robotic transoral periosteal thyroidectomy (TOPOT): experience in two cadavers. J Laparoendosc Adv Surg Tech A 2015;25:139-42. [Crossref] [PubMed]
- Lee HY, You JY, Woo SU, et al. Transoral periosteal thyroidectomy: cadaver to human. Surg Endosc 2015;29:898-904. [Crossref] [PubMed]
- Lee HY, Hwang SB, Ahn KM, et al. The safety of transoral periosteal thyroidectomy: results of Swine models. J Laparoendosc Adv Surg Tech A 2014;24:312-7. [Crossref] [PubMed]
- Inabnet WB 3rd, Suh H, Fernandez-Ranvier G. Transoral endoscopic thyroidectomy vestibular approach with intraoperative nerve monitoring. Surg Endosc 2017;31:3030. [Crossref] [PubMed]
- Park JO, Kim MR, Kim DH, et al. Transoral endoscopic thyroidectomy via the trivestibular route. Ann Surg Treat Res 2016;91:269-72. [Crossref] [PubMed]
- Witzel K, Hellinger A, Kaminski C, et al. Endoscopic thyroidectomy: the transoral approach. Gland Surg 2016;5:336-41. [Crossref] [PubMed]
- Udelsman R, Anuwong A, Oprea AD, et al. Trans-oral Vestibular Endocrine Surgery: A New Technique in the United States. Ann Surg 2016;264:e13-e16. [Crossref] [PubMed]



