Safe implementation of retroauricular robotic and endoscopic neck surgery in South America
Epidemiology and risk factors for head and neck cancer
Cancer is currently a health problem worldwide. Considering all ages, it is the second largest cause of death in the population, falling behind only cardiovascular diseases. Approximately two-thirds of cancer deaths occur in less developed countries, such as the South American countries. The lower chance of long term survival after diagnosis observed in these countries is mainly related to the combination of lack of knowledge, late diagnosis, and limited access to timely and standardized treatment (1).
Around the world, more than 600,000 new cases of head and neck cancer are diagnosed each year, most of them located in the mouth, pharynx, or larynx. In recent years, there has been a significant increase in the incidence of well differentiated thyroid cancer. Upper aerodigestive cancers are more common in men, at the rate of 2–4 cases in men for each case in woman (1-3). Unfortunately, most of the cases are still diagnosed late, when the disease presents at an advanced stage (4), and therefore requires treatment in highly specialized centers. There is great social and economic impact (5), prolonged withdrawal from work, and a lower quality of life of patients and their families. Delayed diagnosis can be attributed to a lack of symptomatic progression in the early stages of the disease, lack of knowledge about cancer, difficulties in accessing the health system, and unprepared health professionals (6,7).
In Brazil, excluding non-melanoma skin cancer (180,000 cases per year), almost 420,000 new cases of cancer were predicted in 2016. The most common locations in the head and neck are: oral cavity, with 11,140 new cases (5.2% of all malignancies diagnosed and 5th most common site in men); larynx, responsible for 6,360 new cases (3.0% of the total and 8th most common site in men); and thyroid gland, with 5,870 new cases (2.9% of the total and the 8th most common site in women) (8).
A.C. Camargo Cancer Center is a tertiary reference center for cancer treatment located in Brazil's largest city, São Paulo, receiving patients from all over the country. The Department of Head and Neck Surgery and Otorhinolaryngology is responsible for approximately 18% of its surgical volume, with more than 2,000 procedures a year, being one of the busiest head and neck services of South America.
Technical evolution literature that motivated the start of head and neck robotic surgery
Robotic surgery was introduced in head and neck oncology approximately 7 years ago, after consolidation of the technique in other areas such as gynecology, cardiothoracic surgery, and, mainly, urology. For some procedures, such as prostatectomy, robotic surgery has become the standard approach. Today, most prostatectomies in the United States are performed by using this technique (9).
Within the last few decades, otolaryngology and head and neck oncologic surgery have shown remarkable progress with the development of several modalities of minimally invasive video assisted surgical procedures (mainly, endonasal, microlaryngoscopic) and improvements in reconstruction techniques. These procedures have resulted in a significant increase in survival and quality of life of the selected treated patients (10). However, extensive approaches and resections are still needed, frequently resulting in aesthetic and functional sequelae with important psychosocial repercussions (11).
Head and neck oncologic surgery is characterized by the manipulation of a highly complex layered anatomy with multiple important (some vital) and delicate structures confined in tight spaces. In addition, it has cavities difficult to access because they are surrounded by bones and cartilage. The traditional surgical approach uses large incisions in visible areas of the human body, frequently resulting in significant aesthetical and functional morbidity. Minimally invasive approaches were not considered an option until a few years ago, because there was concern about visualization and adequate exposure of the tumor. Furthermore, the surgical instruments that facilitate such approaches were rudimentary, not precise, and not readily available (12).
Tumor control and long-term survival are no longer the only major objective of oncological treatment. There has been an increasing concern to reduce morbidity (without jeopardizing oncological safety) and to improve quality of life and patient satisfaction. In recent years, there has been notable progress in minimally invasive video-assisted surgeries associated or not with technological equipment, such as laser and motorized instruments, which could facilitate these procedures (13-15).
Among the most recent advances in head and neck oncology, the use of the Da Vinci system was initiated in 2005 by McLeod and Melder. They performed a resection of a vallecula cyst using the robotic technique. Since then, the evolution of the transoral approach using robotic systems (transoral robotic surgery, TORS) made it eligible for treatment of selected cases of oropharyngeal tumors. In South America, the first TORS was performed by Arap et al. (16). With the use of this technique, a less morbid surgical approach replaced, in selected cases, the need for extensive labial and large transcervical incisions, as well as mandibulotomies, with better functional and aesthetic results, and an acceptable complication rate and comparable oncologic outcomes (15).
It is always important to compare new surgical approaches to the previously reported outcomes from standardized techniques (conventional open technique or endoscopic). The robot offers the surgeon a three-dimensional view and a magnification of the operative field, with several angles of vision. The visualization of depth and the clear discernment of planes and tissues allow small anatomical structures to be distinguished and consequently it reduces the risk of damage (17).
O’Malley et al. reported just a few years ago that enhanced visualization using the robot allowed them to obtain better resections with adequate cancer margins, excellent hemostasis, and easier conservation of important neural structures in resections of tongue tumors via TORS (18). At this point, it is important to make a parallel with the endoscopic technique, which, in spite of also providing smaller and less morbid accesses, requires support points in addition to robust training regarding hand and eye coordination, since the hand goes in the opposite direction of the movement. Robotic surgery allows a better coordination in this aspect, since it accurately portrays the movement performed by the hands. Other important advantages of robotic surgery in the visualization aspect are that there is no need for someone to hold the camera and the surgeon’s autonomy regarding the position of the camera (19). The robot provides camera stability and allows a better range of motion than normal endoscopic surgery (12).
An important aspect concerns the devices and motion delivered by the arms of the robot, especially the precision. The robot’s arms are able to filter out any tremors while transforming large-scale movements into low-amplitude motions. Thus, the dexterity, the motion, and the precision are enhanced. In addition, the arms can carry several instruments that may facilitate certain surgical procedures in anatomical sites difficult to access, such as the use of a laser to treat pharynx and larynx tumors (20). Moreover, the technique is usually comfortable, allowing the surgeon to operate with proper ergonomics. In this way, stress and physical fatigue are minimized and performance is also enhanced (21). Another interesting and promising aspect of the robotic technique concerns the possibility of remote use. Some robots have been created for this purpose, for example for astronauts and soldiers (22). Some studies indicate the potential of robotic surgery to offer the possibility of a physician and patient being geographically separated, in addition to the potential of performing virtual training including training of new surgeons in real situations, treatment planning, and surgical strategies from specific reconstruction software (23).
The use of the Da Vinci robotic surgery system has promoted the development of several surgical approaches with less morbidity and better cosmetic results, including the transaxillary and retroauricular approaches for thyroidectomies, neck dissections, and benign tumor resections (24-32). These tumors have a high incidence worldwide but surgical procedures continue to be performed using only conventional techniques by the majority of head and neck surgeons. Few centers in the western world have significant experience with cervical robotic surgeries, not for lack of equipment, but because of the lack of surgeons trained to use them. Currently, these techniques are more widespread in Asian countries such as Japan, South Korea, and China, because the Asian races have a greater propensity to develop hypertrophic scarring, and consequently the patients are more motivated to avoid a visible neck incision.
Kim et al. in 2014 reported the results of a series of patients with cervical metastases of thyroid neoplasia undergoing neck dissection. The study evaluated 47 patients and compared the open technique with robot-assisted techniques. The results showed a longer operative time for patients undergoing the robotic technique but the degree of aesthetic satisfaction was higher in the robotic surgery group. There was no difference in the number of retrieved lymph nodes or in the incidence of complications. These results suggest that this is a safe technique, with a superior aesthetic result and with similar oncological results. Obviously there is a need for further analysis with a comparison of long-term survival results to actually conclude that it is oncologically adequate, but preliminary results suggest that it is adequate (33).
A recent systematic review evaluating 11 studies demonstrated that as compared to conventional thyroidectomy, robotic thyroidectomy is safe, with similar complication rates (although there is a risk of new and different complications) and better aesthetic results (34). Recent studies demonstrate that thyroidectomy with neck dissection through transaxillary access using the Da Vinci system has similar oncological results compared with classic procedures, with lower rates of postoperative pain, sensory changes in the neck, and swallowing discomfort, and in addition aesthetically more favorable results with no visible cervical scar (29,34). It is important to mention that during the development of minimally invasive transaxillary thyroidectomy, some cases of brachial plexus injury were described, which discouraged some services from initiating such an approach (35).
The reported complications of the transaxillary approach, although infrequent, led to the development of a new modified retroauricular approach, which is a more familiar anatomical area for head and neck surgeons because neck dissection is one of the most common surgical procedures performed by these specialists. Neck dissections can be selective or radical and generally are performed through large cervical incisions that result in significant aesthetic and functional sequels. However, using robotic surgery, these procedures can be performed by retroauricular access with similar results regarding the number of retrieved lymph nodes (oncological safety), but with fewer complications and more favorable cosmetic results (28,29,32,36,37).
Among the advantages of the retroauricular approach, besides the aesthetics, is the greater safety of this incision in comparison to the classic neck dissection incisions in the event of complications such as cutaneous flap necrosis or dehiscence, since the retroauricular incision is not in an area usually included in the radiotherapy fields and its dehiscence or partial loss of the skin flap does not cause exposure of the large cervical vessels and consequently does not increase the risk of bleeding (28). Further follow-up analyzes are necessary to determine oncologic efficacy and to evaluate functional outcomes of these procedures.
In regards to the postoperative complications of neck dissection through the retroauricular approach, some studies are emerging with encouraging results. In 2014, Tae et al. evaluated the feasibility and efficacy of assisted robot neck dissection when compared to the conventional technique in patients with upper aerodigestive tract epidermoid carcinoma (UATEC). Thirty patients with UATEC with clinically negative neck (cN0) underwent selective neck dissection. Eleven patients underwent a retroauricular approach assisted by the robot and 19 patients underwent conventional neck dissection. The mean age was lower in the robotic group (P=0.03); however, sex and TNM stage distribution did not differ between the two groups. Selective neck dissection assisted by the robot was successfully completed in all cases. The mean surgical time was longer in the robotic group (215±56 min) than in the conventional group (144±43 min) (P<0.001). The mean number of lymph nodes removed were 25.0±7.4 and 28.9±8.2 in the robotic and conventional groups, respectively (P=0.192), and the number of resected lymph nodes at each level also did not differ between the two groups. In addition, there was no significant difference in the incidence of postoperative complications between the two groups, but the aesthetic satisfaction was higher in the robot group (P=0.002). Thus, the conclusion is that neck dissection assisted by a robot is comparable to conventional methods in selected patients (32).
Similarly, another Korean group in 2012 published results of an analysis of selective neck dissection. Twenty-six patients with clinically negative neck with oral cavity squamous cell carcinoma were divided into two groups: robot-assisted neck dissection and conventional neck dissection via cervical incision. The results showed that the operation time, amount and duration of drainage, length of hospitalization, complications, and number of dissected lymph nodes were comparable and did not present statistical differences. The mean length of operation was higher in the robot-assisted group (157±22 min) when compared to the conventional group (78±16 min) (P<0.001). However, the degree of satisfaction was significantly higher in the robot-assisted group (P<0.001) (26).
Another type of approach that has been carried out is the treatment of parotid tumors. Resection of parotid tumors with neck dissection can also be performed using the Da Vinci system by retroauricular access with preauricular extension, avoiding a cervical incision. However, the accumulated experience is still limited and there is a need for a greater number of publications to assess the safety of this procedure (30). Benign cervical tumor resection and tumors of the submandibular gland can also be performed with the robotic system through retroauricular access, with similar safety and better aesthetic and functional results (36).
Clearly, the role of robotic surgery in head and neck oncology has been growing and consolidating in recent years, opening up new surgical alternatives to be offered to patients with cancer in these topographies. This process is ongoing with the diffusion of these techniques and technologies in different parts of the world with different degrees of enthusiasm. It will probably increase with the development of robots with systems better adapted to the anatomical peculiarities of the upper aerodigestive tract, base of the skull, and the neck. In the near future, these technologies will be increasingly used in cancer treatment at tertiary referral centers and one of the biggest challenges to be faced is the preparation of a new generation of surgeons better adapted to the technologies to come.
Difficulties for technology adoption in South America
The first major difficulty faced by South American countries is the political-monetary issue. Most of the countries in this large area have fragile public health systems that are lacking in even some basic aspects, so the implementation of expensive technologies to be used in a very selected group of patients is regarded as difficult and not considered to be a priority. In Brazil, there is a mixed system, where most of the country’s population depends entirely on the public system, which cannot keep up with the technological advances made over the years. For the implementation of a new technology, it is necessary to have an adequate financial structure to invest not only in equipment but also in the training and incentives to professionals. Unfortunately, the absence of this aspect is very common and ultimately discourages potential professionals who are responsible for the protagonism and implementation of new techniques and technologies acquired in other countries.
There are many shortcomings in the issue of financial resources, as well as the lack of incentives for the technical preparation of physicians and other health professionals. This set of factors together leads to a significant delay in the South American countries in terms of technological advances. It is necessary to increase the investments and, with that, increase the incentive and qualification of these professionals. Well-designed cost-effectiveness studies need to be implemented so that we can consider what can become routine and what may not be sustainable.
To better understand this scenario we can observe the delay in robotic radical prostatectomy (RRP) adoption across America. In the USA, the first reports of RRP emerged in 2001; from 2003 to 2010, RRP adoption increased from 0.7% to 42% of surgeons performing radical prostatectomy (RP) in the USA. According to the National Institutes of Health, nowadays approximately 80% of RPs are RRPs and the USA has more than 2,500 robotic systems in clinical use. Meanwhile, in Brazil, we had the first RRP only in 2008 (8 years delay when comparing with the USA); nowadays less than 5% of RPs are RRPs and we have just 26 robotic systems in Brazil and another 27 in all of Latin America (37-39). Another clear example of poor technology accessibility in Brazil is that 88% of elective cholecystectomies performed are conventional procedures and only 12% are laparoscopic (40).
Implementation of robotic and endoscopic neck surgery in South America
In 2014, after initial discussion and literature review, we decided to try a retroauricular approach for selected benign tumors, prophylactic selective dissections of levels I–III, and other procedures such as paraganglioma resection and submandibular gland excision. In that phase, we were already receiving on-line tutoring from Prof. Koh, from Yonsei University (Head and Neck Department). Following the first ten successful cases, three head and neck surgeons of our team went to Seoul for further training. This 2-week period consisted of clinical observation of several retroauricular and transaxillary procedures, as well as video sessions and clinical discussions. We also performed a fresh cadaver dissection using a retroauricular robotic-assisted approach for thyroid surgery and neck dissection, under the supervision of Yonsei University's faculty. These three attending surgeons, that were already approved console surgeons by Intuitive Surgical, became certified for neck robotic surgery by Yonsei University.
However, in this initial training process we had to face several obstacles, demanding a significant personal effort by our faculty. First, our institution managers failed to see the importance of these technical innovations and consequently did not provide appropriate support for the initial training steps in Korea. In addition, local representatives of Intuitive Surgery also failed to understand the importance of neck robotic surgery implementation in South America and refused training support for this purpose. Other challenging issues emerged from the impossibility of importing Chung’s retractor for clinical use in Brazil, requiring adaptation of the Bookwalter retractor (used for abdominal surgery) for retroauricular procedures. Nevertheless, we were able to overcome these hurdles and now have tremendous support from our institution after the demonstration of safety and observation of the patients’ satisfaction.
The first retroauricular robotic neck dissection in South America was performed at A.C. Camargo Cancer Center in November 2014. It was preceded by 15 cases of endoscopic-assisted retroauricular procedures including supraomohyoid neck dissections, submandibular gland excisions, hemithyroidectomies, and benign tumor resection. The transition from endoscopic to robotic retroauricular surgery was natural and smooth, without any major setback or additional difficulty when starting to use the Da Vinci Si system to perform those procedures. This transition process was obviously facilitated by our previous experience with TORS using the same robotic system on at least 25 cases (10 performed by one of us at Sirio Libanes Hospital).
For more than 2 years now, both robotic- and endoscopic-assisted retroauricular approaches have been used routinely for selected cases in our department. In this period, we have worked on technical improvements and the learning process. The indications were expanded to thyroid surgery associated with neck dissection and neck dissections including levels I–VI. Nowadays, we perform endoscopic or robotic retroauricular surgery for head and neck carcinomas, thyroid cancer, salivary gland tumors, paragangliomas, thyroglossal cysts, and other benign tumors. During all phases of that implementation, continuous prospective data have been collected and compared to conventional procedures performed in the last 2 years, in order to identify possible increases in complications or decreases in safety compliance.
From June 2014 to December 2016, we have performed a total of 121 retroauricular neck surgeries, of which 65 were robotic-assisted and 56 were endoscopic assisted procedures (Table 1). Here we are not including some procedures that were performed via facelift or a retroauricular approach without the need of special instrumentation assistance, such as parotidectomies or level II neck dissections, performed under simple direct view. In this initial experience, special attention was paid to safety and the complication rate. Looking at the entire sample, we had 5 hematomas that needed reoperation (one in a patient who had developed an orocutaneous fistula and another in a patient with chronic liver disease), 3 surgical site infections treated with antibiotics and needle aspiration, 5 minor skin flap necrosis (<15 mm), 3 transient vocal cord paresis, and 9 marginal branch paresis (Table 1). This complication rate seems to be comparable to conventional procedures in our experience.

Full table
However, we hope that our increasing numbers will allow us to perform matched comparisons of specific procedures in the near future, analyzing also patient satisfaction, oncologic, functional, and aesthetic outcomes. In a recent paper (submitted) we compared early outcomes of conventional (43 patients) versus endoscopic and robotic retroauricular (17 patients) neck dissection for oral cancer, showing similar results considering complication rates (but a longer operative time in the retroauricular group), number of retrieved lymph nodes, and recurrence-free survival.
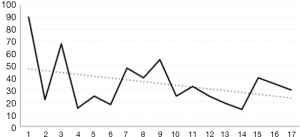
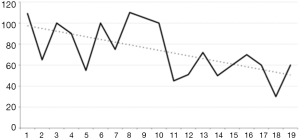
We believe that we are at the end of our learning curve for the most commonly performed procedures, such as thyroid lobectomy and neck dissection. We have become very familiar with the retroauricular approach, and the set up time for both endoscopic and robotic procedures as well as the console time in robotic surgery have decreased significantly, especially after our first 50 cases. Currently, the skin flap dissection takes approximately 15 minutes and the set up time is no more than 5 minutes. Obviously, console time depends on the surgical procedure and also the surgeon’s experience, but in general, our console time has been decreasing for different procedures, as shown in Figures 1 and 2.
Future steps
In the last few years, significant international collaborations between our institute and Yonsei University and other centers experienced in endoscopic and robotic neck surgery have been developed, including on-line experience sharing and creation of the International Guild of Endoscopic & Robotic Head and Neck Surgery (IGERHNS), a research organization comprising surgeons from academic institutions around the globe, with significant expertise in robotic and endoscopic procedures, dedicated to promoting sharing of data and best practices for high-quality collaboration. This guild had its first meeting in 2015 and the next two are already scheduled for 2017 (Switzerland) and 2018 (Brazil). In addition, the members have gathered together for discussions, including at head and neck conferences and robotic surgery meetings.
The A.C. Camargo Cancer Center is a reference center for cancer treatment, research, and education in South America. We have a residency program on head and neck surgery (designed for Brazilian general surgeons) and an advanced fellowship training program for which most of the applicants are from other South American countries. One of our early goals is to include retroauricular endoscopic training in these programs, possibly creating a specific fellowship for endoscopic and robotic head and neck surgery, and also to promote focused short-term courses for head and neck surgeons from other institutions, starting in 2017. Development of lab models that would facilitate such a teaching process is extremely important, especially in countries where access to cadaver dissection is difficult or too expensive.
Despite the current lack of a formal training model in our institution, two of our former fellows from other countries in South America are already performing retroauricular endoscopic surgeries, but are still at the beginning of their learning curves. Another important step in encouraging more South American surgeons to adopt endoscopic and robotic neck surgery is to propagate our experience with publications and congress presentations showing the operative technique and results. Last year, we published two papers (41,42) (another three are currently in the publication process) and we presented at more than 15 congresses on this subject. However, this is not an easy task as the local medical journals have low impact factors and most of our data represents an initial reproduction of a much larger experience already well described in the literature, especially by Korean authors (17,25,26,28,30,32,43,44).
As expected, the implementation and acceptance of new technologies is not a simple and steady process. The “chasm” placed between the technology adoption by innovators or early adopters and the majority of users is well-known in the marketing literature and has been described in the book Crossing the Chasm by Geoffrey A. Moore, 1999 (45). This can be easily translated to the resistance that the innovators and early adopters of neck endoscopic and robotic surgery face when discussing this evolution with their peers who are not yet convinced to accept it.
Crossing this “chasm” is the ultimate challenge for making endoscopic and robotic neck surgery widely accepted and adopted. Accomplishment of this goal would demand a great effort to obtain and publish strong, objective, clear and reproducible data establishing the advantages of these techniques.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [Crossref] [PubMed]
- Chaturvedi AK, Anderson WF, Lortet-Tieulent J, et al. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol 2013;31:4550-9. [Crossref] [PubMed]
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893-917. [Crossref] [PubMed]
- Tanriover O, Hidiroglu S, Save D, et al. Knowledge of oral cancer, preventive attitudes, and behaviors of primary care physicians in Turkey. Eur J Cancer Prev 2014;23:464-8. [Crossref] [PubMed]
- Wineland AM, Stack BC. Modern methods to predict costs for the treatment and management of head and neck cancer patients: examples of methods used in the current literature. Curr Opin Otolaryngol Head Neck Surg 2008;16:113-6. [Crossref] [PubMed]
- Kowalski LP, Franco EL, Torloni H, et al. Lateness of diagnosis of oral and oropharyngeal carcinoma: factors related to the tumour, the patient and health professionals. Eur J Cancer B Oral Oncol 1994;30B:167-73. [Crossref] [PubMed]
- LeHew CW, Epstein JB, Koerber A, et al. Training in the primary prevention and early detection of oral cancer: pilot study of its impact on clinicians’ perceptions and intentions. Ear Nose Throat J 2009;88:748-53. [PubMed]
- National Cancer Institute - Brazil. Estimate cancer incidence in Brazil 2016. Retrieved January 15, 2017. Available online: http://www.inca.gov.br/estimativa/2016/estimativa-2016-v11.pdf
- Dasgupta P, Kirby RS. The current status of robot-assisted radical prostatectomy. Asian J Androl 2009;11:90-3. [Crossref] [PubMed]
- Dziegielewski PT, Teknos TN, Durmus K, et al. Transoral robotic surgery for oropharyngeal cancer: long-term quality of life and functional outcomes. JAMA Otolaryngol-- Head Neck Surg 2013;139:1099-108. [Crossref] [PubMed]
- Weymuller EA, Yueh B, Deleyiannis FW, et al. Quality of life in patients with head and neck cancer: lessons learned from 549 prospectively evaluated patients. Arch Otolaryngol Head Neck Surg 2000;126:329-35. [Crossref] [PubMed]
- Brunaud L, Germain A, Zarnegar R, et al. Robotic thyroid surgery using a gasless transaxillary approach: cosmetic improvement or improved quality of surgical dissection? J Visc Surg 2010;147:e399-402. [Crossref] [PubMed]
- Fan S, Liang FY, Chen WL, et al. Minimally invasive selective neck dissection: a prospective study of endoscopically assisted dissection via a small submandibular approach in cT(1-2_N(0) oral squamous cell carcinoma. Ann Surg Oncol 2014;21:3876-81. [Crossref] [PubMed]
- Ozer E, Alvarez B, Kakarala K, et al. Clinical outcomes of transoral robotic supraglottic laryngectomy. Head Neck 2013;35:1158-61. [Crossref] [PubMed]
- van Loon JW, Smeele LE, Hilgers FJ, et al. Outcome of transoral robotic surgery for stage I-II oropharyngeal cancer. Eur Arch Otorhinolaryngol 2015;272:175-83. [Crossref] [PubMed]
- Arap SS, Moyses RA, Brandão LG, et al. Câncer de faringe tratado com tonsilectomia radical transoral por cirurgia robótica. Rev Bras Cir Cabeça Pescoço 2009;38:54-5.
- Kim KH, Choi HG JY. Head and neck robotic surgery: pros and cons [Internet]. Head and neck robotic surgery: pros and cons. Head Neck Oncol 2013;5:26. 2013 [cited 2014 May 11]. Available online: http://www.oapublishinglondon.com/images/article/pdf/1366478462.pdf
- O’Malley BW, Weinstein GS, Snyder W, et al. Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope 2006;116:1465-72. [Crossref] [PubMed]
- Alessandrini M, De Padova A, Napolitano B, et al. The AESOP robot system for video-assisted rigid endoscopic laryngosurgery. Eur Arch Otorhinolaryngol 2008;265:1121-3. [Crossref] [PubMed]
- Kim VB, Chapman WH, Albrecht RJ, et al. Early experience with telemanipulative robot-assisted laparoscopic cholecystectomy using da Vinci. Surg Laparosc Endosc Percutan Tech 2002;12:33-40. [Crossref] [PubMed]
- Berguer R, Smith W. An ergonomic comparison of robotic and laparoscopic technique: the influence of surgeon experience and task complexity. J Surg Res 2006;134:87-92. [Crossref] [PubMed]
- Camarillo DB, Krummel TM, Salisbury JK. Robotic technology in surgery: past, present, and future. Am J Surg 2004;188:2S-15S. [Crossref] [PubMed]
- Feifer A, Al-Ammari A, Kovac E, et al. Randomized controlled trial of virtual reality and hybrid simulation for robotic surgical training. BJU Int 2011;108:1652-6. [Crossref] [PubMed]
- Blanco RG, Boahene K. Robotic-assisted skull base surgery: preclinical study. J Laparoendosc Adv Surg Tech A 2013;23:776-82. [Crossref] [PubMed]
- Byeon HK, Holsinger FC, Koh YW, et al. Endoscopic supraomohyoid neck dissection via a retroauricular or modified facelift approach: preliminary results. Head Neck 2014;36:425-30. [Crossref] [PubMed]
- Lee HS, Kim WS, Hong HJ, et al. Robot-assisted Supraomohyoid neck dissection via a modified face-lift or retroauricular approach in early-stage cN0 squamous cell carcinoma of the oral cavity: a comparative study with conventional technique. Ann Surg Oncol 2012;19:3871-8. [Crossref] [PubMed]
- Lee J, Chung WY. Robotic thyroidectomy and neck dissection: past, present, and future. Cancer J 2013;19:151-61. [Crossref] [PubMed]
- Park YM, Holsinger FC, Kim WS, et al. Robot-assisted selective neck dissection of levels II to V via a modified facelift or retroauricular approach. Otolaryngol Head Neck Surg 2013;148:778-85. [Crossref] [PubMed]
- Seup Kim B, Kang KH, Park SJ. Robotic modified radical neck dissection by bilateral axillary breast approach for papillary thyroid carcinoma with lateral neck metastasis. Head Neck 2015;37:37-45. [Crossref] [PubMed]
- Shin YS, Choi EC, Kim CH, et al. Robot-assisted selective neck dissection combined with facelift parotidectomy in parotid cancer: Robotic Neck Dissection for Parotid Cancer. Head Neck 2014;36:592-5. [Crossref] [PubMed]
- Sun GH, Peress L, Pynnonen MA. Systematic review and meta-analysis of robotic vs conventional thyroidectomy approaches for thyroid disease. Otolaryngol Head Neck Surg 2014;150:520-32. [Crossref] [PubMed]
- Tae K, Ji YB, Song CM, et al. Robotic selective neck dissection by a postauricular facelift approach: comparison with conventional neck dissection. Otolaryngol Head Neck Surg 2014;150:394-400. [Crossref] [PubMed]
- Kim WS, Koh YW, Byeon HK, et al. Robot-assisted neck dissection via a transaxillary and retroauricular approach versus a conventional transcervical approach in papillary thyroid cancer with cervical lymph node metastases. J Laparoendosc Adv Surg Tech A 2014;24:367-72. [Crossref] [PubMed]
- Lee J, Kwon IS, Bae EH, et al. Comparative Analysis of Oncological Outcomes and Quality of Life After Robotic versus Conventional Open Thyroidectomy With Modified Radical Neck Dissection in Patients With Papillary Thyroid Carcinoma and Lateral Neck Node Metastases. J Clin Endocrinol Metab 2013;98:2701-8. [Crossref] [PubMed]
- Davis SF, Abdel Khalek M, Giles J, et al. Detection and prevention of impending brachial plexus injury secondary to arm positioning using ulnar nerve somatosensory evoked potentials during transaxillary approach for thyroid lobectomy. Am J Electroneurodiagnostic Technol 2011;51:274-9. [PubMed]
- Lee HS, Lee D, Koo YC, et al. Endoscopic resection of upper neck masses via retroauricular approach is feasible with excellent cosmetic outcomes. J Oral Maxillofac Surg 2013;71:520-7. [Crossref] [PubMed]
- Chang SL, Kibel AS, Brooks JD, et al. The impact of robotic surgery on the surgical management of prostate cancer in the USA. BJU Int 2015;115:929-36. [Crossref] [PubMed]
- Intuitive Surgical, Inc. - da Vinci Surgical System [Internet]. [cited 2017 Jan 13].
- Tracking the Rise of Robotic Surgery for Prostate Cancer - National Cancer Institute [Internet]. [cited 2017 Jan 13]. Available online: https://www.cancer.gov/about-cancer/treatment/research/rise-robotic-surgery
- Castro PM, Akerman D, Munhoz CB, et al. Laparoscopic cholecystectomy versus minilaparotomy in cholelithiasis: systematic review and meta-analysis. Arq Bras Cir Dig 2014;27:148-53. [Crossref] [PubMed]
- Lira RB, Chulam TC, Koh YW, et al. Retroauricular Endoscope-Assisted Approach to the Neck: Early Experience in Latin America. Int Arch Otorhinolaryngol 2016;20:138-44. [Crossref] [PubMed]
- Chulam TC, Lira RB, Kowalski LP. Robotic-assisted modified retroauricular cervical approach: initial experience in Latin America. Rev Col Bras Cir 2016;43:289-91. [Crossref] [PubMed]
- Lee J, Chung WY. Robotic Surgery for Thyroid Disease. Eur Thyroid J 2013;2:93-101. [PubMed]
- Choi EC, Koh YW. Endoscopic and Robotic Neck Surgery. Seoul: Joo Sub Song, 2013:141.
- Moore GA. Crossing the chasm: marketing and selling high-tech products to mainstream customers. New York: HarperBusiness, 1999.