Neck ultrasonography for detection of non-recurrent laryngeal nerve
Introduction
The inferior laryngeal nerve is a branch of the vagus nerve that supplies all the intrinsic muscles of the larynx with the exception of the cricothyroid muscles; it includes also sensitive fibers to the subglottal part of the larynx, cardiac branches to the deep cardiac plexus, and branches to the trachea, esophagus and the inferior constrictor muscles. For this reason, it is fundamental in phonatory and respiratory functions and swallowing.
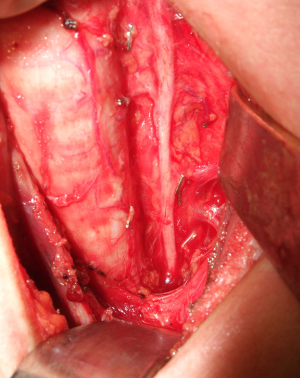
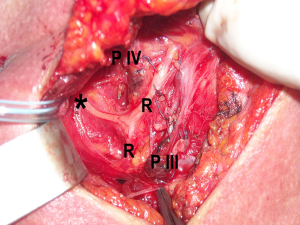
It originates from the vagus nerve at the level of the mediastinum to follow its recurrent route ascending to laryngeal entry point (Figures 1,2) (1). Rarely, it may arise from the vagus nerve at the level of the neck to take a non-recurrent course (Figure 3).
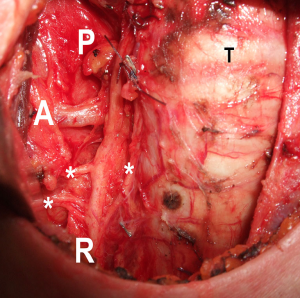

The non-recurrent laryngeal nerve (NRLN) is a rare anatomical variant; it occurs rarely on the right side, while it is exceptional on the left side (2); different types of non-recurrent courses have been described (3). NRLN is associated with vascular anomalies of the aortic arches due to embryologic reasons. On the right side, it is associated to the absence of the brachiocephalic trunk; in this condition, the common carotid artery arises from the aortic arch and the right subclavian artery has an aberrant course (lusorian artery) (2,4-7). This anomaly is reported with a widely variable prevalence (0.3–6%) in literature (2,4-8).
Because of its anatomic position, NRLN represents an important risk factor of injury and subsequent vocal cord paralysis during neck surgery. Thus, its early recognition is crucial (9-12).
The intraoperative identification and preservation of NRLN is a challenging procedure: this nerve with an unusual course may be misdiagnosed and damaged during neck surgical procedures, even by experienced surgeons. The availability of a preoperative diagnosis of NRLN may reduce the risk of accidental nerve injuries (9-12).
Several imaging techniques have been proposed for the preoperative identification of NRLN including chest X-ray, barium swallowing test, Computed Tomography (CT), Magnetic Resonance (MR), esophageal endoscopy, and intraoperative neuromonitoring (IONM), but their routine use is limited by the variable diagnostic accuracy, invasiveness, and costs. Recently, ultrasonography (US) has been suggested as a simple, effective, and reliable diagnostic tool (9), since it may easily detect the associated arterial abnormalities, i.e., the absence of the brachiocephalic trunk and/or the presence of the lusorian artery.
Literature concerning the neck US, as a tool for detection of NRLN is relatively scarce. The aim of this paper is to review the literature, in order to offer an up to-date on this technique and its results.
Methods
A web search, focusing on humans, was performed by PubMed database, including papers published up to 20 August 2016, using the key words “ultrasonography” AND “non-recurrent laryngeal nerve” or “nonrecurrent laryngeal nerve”. A total of 13 papers were found. The bibliographic search evaluated also the related references cited by the above-mentioned papers; in case of multiple publications from the same authors or institutions, only the latest and largest series were considered, in order to avoid the duplication of cases.
Results
After the review process and exclusion of inappropriate or duplicated papers, eight papers were selected (9,13-19). They included more than 17,873 patients; among them, 3,740 patients underwent neck US for the detection of NRLN. At surgery, the incidence of NRLN varied between 0.4% and 1.94%. Five studies focused on the preoperative use of US (13,15-17,19). The sensitivity and specificity of US varied between 99–100% and 41–100%, respectively. The results are summarized in the Table 1.

Full table
The first study was published in 2003 by Devèze et al. (9), who postulated that cervical duplex scanning of the brachiocephalic artery could identify patients at risk of a NRLN. Twelve patients with an operative diagnosis of a right NRLN underwent postoperative US. They used transducers of 3.5 or 7.5 MHz, according to the thickness of the patient’s subcutaneous tissue. The examination consisted in following the right common carotid artery from the neck to the aortic arch, searching the division of the brachiocephalic artery into the right common carotid artery and the right subclavian artery. The average time of the assessment was 5 min (range, 3–10 min); the Authors concluded that duplex scanning could be a reliable and noninvasive tool to identify arterial abnormalities, with a positive predictive value of the presence on NRLN of 100%.
In 2010 Huang and Wu (13) proposed a preoperative neck US using both 3.5 and 10 MHz probes, in 2,330 patients undergoing thyroidectomy to check the absence of brachiocephalic artery, defined as predictive of right NRLN. Thirteen positive patients were found by 10-MHz probe; of those 11 were also identified by 3.5-MHz probe, and proved to be carrier of a right NRLN at surgery. The two false-positive patients found by 10-MHz probe were due to short and tortuous innominate artery, respectively. The neck US sensitivity and specificity for predicting NRLN was 100% when a 3.5-MHz probe was used, while it was 100% and 99%, respectively, when a 10 MHz probe was used.
In 2011 an Italian group (14) reviewed 2,713 total thyroidectomies and found a NRLN in 17 patients. Postoperative US and MR were performed in 15 patients and in two cases no abnormalities could be identified by either imaging technique; the diagnostic sensitivity of US was 84.6%.
The prospective study of Yetisir et al. (15) included 332 patients who underwent thyroidectomy or parathyroidectomy. Preoperative US was performed in all patients to identify vascular anomalies related to NRLN; CT was performed only in patients with positive US. The NRLN was identified in six patients on the right side and preoperative US predicted NRLN in all cases (overall accuracy 100%).
In 2013, a Japanese group (16) evaluated the usefulness of CT and US for preoperative diagnosis of the NRLN. They reviewed 1,561 patients who underwent thyroid surgery and found 11 NRLN. The sensitivity and specificity of CT for detection of the NRLN was 100% for both. On the other hand, preoperative US detected the bifurcation of the brachiocephalic trunk in 116 of 140 patients; the bifurcation in the remaining patients was not detectable, but at surgery a NRLN was found only in one out of the 24 patients. Thus, the sensitivity and specificity of cervical US in detecting the right-sided NRLN was 100% and 83.5%, respectively.
In 2014, Wang et al. (17) reviewed preoperative chest X-rays, US, and CT of 5 patients with NRLN. Preoperative CT predicted NRLN in all 5 cases (100% accuracy). They found no predictive features of NRLN at chest X-ray and US before surgery. However, by reviewing the preoperative US images they found that the brachiocephalic truck was absent in all patients.
The same year, Yang et al. (18) tried to determine the value of chest X-ray and cervical US in predicting the presence of NRLN. Their study included 2,251 patients that underwent surgery for various thyroid disease. Chest X-ray found 49 patients with suspected NRLN, confirmed during operation in 23 cases. In the 2,202 unsuspected cases, five had NRLN during surgeries. Aberrant subclavian arteries were found in postoperative US in all 28 cases of NRLN confirmed during surgery.
In 2015, Iacobone et al. (19) examined 1,477 patients undergoing thyroid and parathyroid surgery with right-side inferior laryngeal nerve exploration. The results of 878 patients that underwent preoperative US (pUS group) were compared with those from a control group of 599 patients that did not perform the exam before surgery. The preoperative US was performed by a linear transducers of 5 to 10 MHz. The NRLN detection was significantly higher in patients of pUS group than controls (1.9% vs. 0.6%, respectively, P<0.05). Moreover, pUS predicted NRLN in all cases and the overall laryngeal nerves morbidity was significantly lower in the pUS group than controls (1.8% vs. 4.2%, respectively, P<0.05). The absence of the brachiocephalic trunk (named “Y sign”) was highly sensitive (sensitivity and negative predictive value, 100%) in predicting the lack of the brachiocephalic trunk and the presence of a NRLN; false positive results occurred in obese patients and large mediastinal goiters. Conversely, the direct origin of the common carotid artery from the aortic arch at pUS had a specificity of 100% and a sensitivity of 41.1%.
Discussion
NRLN is a rare finding that occurs most often on the right side (0.3–6% of cases), whereas it is exceptional on the left side (0.04%) (2,4-7). When a NRLN is misdiagnosed, it is exposed to increased risk of injury during neck surgery. In fact, a recent study (19) found a significantly increased rate of nerve injuries in patients with right NRLN compared to normal recurrent laryngeal nerve (14.3% vs. 1.75%) during thyroid and parathyroid surgery.
The presence of a right NRLN is the consequence of a vascular anomaly: the right subclavian artery does not arise from the brachiocephalic artery, but directly from the aortic arch in distal position respect of the origin of the left subclavian artery. This anomaly was first described by Bayford in 1789 in a patient with secondary dysphagia linked to an intertracheo-esophageal course of the right subclavian artery (20). Subsequently, in 1936, Arkin named this artery placed in abnormal position ‘‘arteria lusoria’’ (21).
The NRLN, instead, was described for the first time during a necropsy, by Stedman in 1823 (22). He found a ‘‘right inferior laryngeal nerve in a non-recurrent situation’’ associated with a right subclavian artery in an abnormal position behind the esophagus, and proposed a relationship between the findings.
Thus, the absence of the brachiocephalic artery, due to an anomaly in embryologic development of the primitive aortic arches, is connected to the nervous anomaly.
During early embryonic development, the recurrent laryngeal nerve is dragged down into the mediastinum and recurs around the sixth primitive aortic arch. On the left side, it recurs around the arterial ligament, at its origin from the aortic arch. On the right side, following the regression of the fifth and sixth arch, it recurs around the fourth primitive aortic arch (i.e., the origin of the subclavian artery from the brachiocephalic trunk). In case of regression of the fourth aortic arch, the NRLN is free to migrate upward. Thus, it reaches the larynx directly from the vagus nerve at a cervical level, with a transverse, non-recurrent course; the brachiocephalic artery is absent and the common carotid artery originates directly from the aortic arch; thus, the right subclavian artery originates from the aortic arch below the left subclavian artery and reaches the right axilla, crossing the mediastinum with a retroesophageal course; in some case it may have a pretracheal or intertracheo-esophageal course (2,23). On the left side, a situs viscerum inversus with dextrocardia, a right-positioned aortic arch, the regression of the arterial ligament, and a left aberrant subclavian artery with a lusorian course are necessary to obtain a left NRLN; subsequently, the anomaly is expected to be extremely rare.
Several anatomical classifications of NRLN have been proposed. In 1972 Stewart et al. (24) described two types of NRLN as horizontal (type I) and descending (type II).
Recently Hong et al. (25) proposed a classification of NRLN based on its travelling pattern: descending (the nerve descends from the vagus nerve trunk); vertical (the nerve runs vertically to the cricothyroid joint); ascending (the nerve runs upward to the cricothyroid joint); and V-shaped (the nerve takes a downward course and runs upward to the cricothyroid joint).
However, NRLN may be underestimated because it may be missed or misdiagnosed (26,27). In fact, in the recent study of Iacobone et al. (19) the overall rate of unidentified inferior laryngeal nerve during surgery was significantly higher in patients that did not perform preoperative US than those undergoing this search (2.67% vs. 1.14%, respectively), suggesting that NRLN could be missed if surgeons are not alerted to this possibility. Furthermore, a false recurrent laryngeal nerve (i.e., nerve branch ascending from the sympathetic stellate ganglion) may be misinterpreted as true recurrent laryngeal nerve, whereas the concomitant NRLN might be missed if there is no preoperative suspicion. On the contrary, large transverse anastomotic branches between the cervical sympathetic trunk and the larynx may simulate a NRLN without arterial abnormalities (Figure 4) (19,28,29).
Several techniques for preoperative identification of this anomaly have been proposed (chest X-ray, barium swallowing test, CT, MR, esophageal endoscopy, and IONM) (7,11,14-18,23,30-32) but their routine use is limited by the variable diagnostic accuracy, invasiveness, and costs.
All these tests are aimed to detect not the NRLN, but the associated abnormalities of the epiaortic vessels (absence of the brachiocephalic trunk and present of a lusorian artery), that are associated with the presence of NRLN in almost 100% of cases.
In less than 20% of cases, chest X-ray can reveal an oblique linear shadow on frontal view and a rounded image from the aortic arch to right and upward (2,17-18,31). Thus, because of the low accuracy, this examination cannot be recommended to predict the presence of a NRLN.
The barium swallowing test may demonstrate a compression on the left edge of the posterior esophagus notch, below the aortic arch (the bayonet sign), caused by the presence of the retroesophageal lusorian artery (Figure 5); however, this sign can be missed if lateral or oblique views are not performed (2,23). Otherwise, this technique is not cost-effective and exposes the patient to X-rays to search an indirect sign.

Esophagoscopy has been reported to detect an extrinsic and pulsating compression of esophageal wall caused by the presence of an aberrant right subclavian artery in 40% of patients with NRLN (23,32); endoscopic ultrasound can demonstrate the presence of this artery in all cases, but its use is limited by invasiveness and costs (23,32).
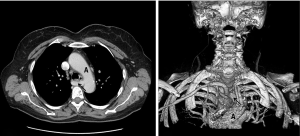
CT and MR can demonstrate directly the presence of the lusorian artery and the absence of the brachiocephalic trunk (Figure 6) (10,14-17). Furthermore, they can be performed before thyroid and parathyroid surgery to evaluate intrathoracic goiters, in staging cancers, or in other selected cases. However, technical reasons can cause the missing of brachiocephalic trunk in CT studies, in approximately 75% of cases (33). Moreover, even if present, the final report usually does not describe the vascular abnormalities in 80% of cases, especially when the thorax and the mediastinum are not the target of the study (7).
The main limits to the systematic use of all these preoperative techniques for the detection of NRLN are the variable accuracy, the invasiveness, and the costs. Moreover, the NRLR is a very rare situation. Thus, to date, the preoperative diagnosis of a NRLN is available only in a percentage ranging between 6% and 24% (2,5). For these reasons, the systematic search and careful dissection of the inferior laryngeal nerve is still the main suggested method to avoid nerve injuries (2).
In recent years, IONM is becoming a common practice in thyroid and parathyroid surgery because, through vagal stimulation, it makes easier to identify the recurrent and non-recurrent laryngeal nerve and verify their functional integrity. In fact, a positive electromyographic response to the proximal stimulation of the vagus (at the superior border of thyroid cartilage) and the absence of response to its distal stimulation (below the inferior border of the fourth tracheal ring) reliably identify a NRLN and this is helpful for the surgeon to optimize the dissection (30). However, IONM is not ubiquitously available; it is still considered not cost-effective in some surgical setting (1,8,30).
US can be considered a rapid, non-invasive and cost-effective tool to detect a NRLN according to the presence of epiaortic vascular abnormalities, with an overall accuracy >98% (9,13,15-19,29). It may be used preoperatively and may alert the surgeon about this occurrence; thus, a focused strategy may be used during surgery to minimize any risk of nerve injuries. It may represent a cost-effective strategy since the neck vascular anatomy exploration can easily complete the thyroid or parathyroid assessment, which is often performed directly by the surgeon in the immediate preoperative period.
Preoperative US can be performed by high-resolution linear array transducers of 5 to 10 MHz; some Authors use transducer of 3.5 or 7.5 MHz (9); 3.5-MHz convex probe and 10-MHz linear probe (13) or linear array transducers 3.6–13.1 and 1.8–6.2 MHz curved array, for infraclavicular region (15). The technique has been extensively reported by Iacobone (19,29), who proposed to place the patient in a supine position with mild hyperextension and left extra rotation of the neck. After the identification of the right common carotid artery at neck level, the transducer can be angled downward at the sternal notch to follow its course from the neck to its origin. Usually, the right common carotid and the right subclavian artery arise together from the bifurcation of the brachiocephalic artery, describing a Y, which has been named “Y sign” [Figure 7 (left)]. When the bifurcation is not recognized, the course of the right common carotid artery can be traced to identify its direct origin from the aortic arch, associated with a right subclavian artery arising independently [Figure 7 (right)]. The Color Doppler tool can be used for a better identification of the vessels.
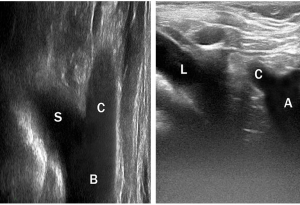
The presence of a “Y sign” may predict a normal vascular and nervous anatomy in virtually all patients (19,29). To the contrary, the presence of a lusorian artery may predict a NRLN in 100% of cases, but the direct US exploration of the origin of an aberrant right subclavian artery can be reported in a minority of cases, since it is technically challenging, because of its deep location in the mediastinal region (19,29). Moreover, the “Y sign” can be falsely absent also in some patients without NRLN, since a normal brachiocephalic trunk cannot be easily detected at US in obese patients and large goiters. In fact, in these situations, the mediastinal region cannot be exhaustively explored by US; thus, CT and MR may be required to confirm locoregional anatomy and plan the surgical strategy.
Conclusions
US is a simple, non-invasive and cost-effective method to detect NRLN (according to the absence of the “Y sign”), since these abnormalities are associate in almost all cases. This tool may be used preoperatively and may prevent the intraoperative nerve damage, since the risk of NRLN palsies is significantly reduced when a preoperative diagnosis is available. However, the accuracy of this strategy is not absolute, since some false positive and negative cases may occur because of difficult US access to mediastinal vascular anatomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Brauckhoff M, Machens A, Sekulla C, et al. Latencies shorter than 3.5 ms after vagus nerve stimulation signify a nonrecurrent inferior laryngeal nerve before dissection. Ann Surg 2011;253:1172-7. [Crossref] [PubMed]
- Henry JF, Audiffret J, Denizot A, et al. The nonrecurrent inferior laryngeal nerve: review of 33 cases, including two on the left side. Surgery 1988;104:977-84. [PubMed]
- Weiand G, Mangold G. Variations in the course of the inferior laryngeal nerve. Surgical anatomy, classification, diagnosis. Chirurg 2004;75:187-95. [Crossref] [PubMed]
- Avisse C, Marcus C, Delattre JF, et al. Right nonrecurrent inferior laryngeal nerve and arteria lusoria: the diagnostic and therapeutic implications of an anatomic anomaly. Review of 17 cases. Surg Radiol Anat 1998;20:227-32. [Crossref] [PubMed]
- Defechereux T, Albert V, Alexandre J, et al. The inferior non recurrent laryngeal nerve: a major surgical risk during thyroidectomy. Acta Chir Belg 2000;100:62-7. [PubMed]
- Proye CA, Carnaille BM, Goropoulos A. Nonrecurrent and recurrent inferior laryngeal nerve: a surgical pitfall in cervical exploration. Am J Surg 1991;162:495-6. [Crossref] [PubMed]
- Hermans R, Dewandel P, Debruyne F, et al. Arteria lusoria identified on preoperative CT and nonrecurrent inferior laryngeal nerve during thyroidectomy: a retrospective study. Head Neck 2003;25:113-7. [Crossref] [PubMed]
- Donatini G, Carnaille B, Dionigi G. Increased detection of non-recurrent inferior laryngeal nerve (NRLN) during thyroid surgery using systematic intraoperative neuromonitoring (IONM). World J Surg 2013;37:91-3. [Crossref] [PubMed]
- Devèze A, Sebag F, Hubbard J, et al. Identification of patients with a non-recurrent inferior laryngeal nerve by duplex ultrasound of the brachiocephalic artery. Surg Radiol Anat 2003;25:263-9. [Crossref] [PubMed]
- Materazzi G, Berti P, Iacconi P, et al. Nonrecurrent laryngeal nerve predicted before thyroidectomy by preoperative imaging. J Am Coll Surg 2000;191:580. [Crossref] [PubMed]
- Watanabe A, Kawabori S, Osanai H, et al. Preoperative computed tomography diagnosis of non-recurrent inferior laryngeal nerve. Laryngoscope 2001;111:1756-9. [Crossref] [PubMed]
- Nagayama I, Okabe Y, Katoh H, et al. Importance of pre-operative recognition of the nonrecurrent laryngeal nerve. J Laryngol Otol 1994;108:417-9. [Crossref] [PubMed]
- Huang SM, Wu TJ. Neck ultrasound for prediction of right nonrecurrent laryngeal nerve. Head Neck 2010;32:844-9. [PubMed]
- Tartaglia F, Blasi S, Tromba L, et al. Duplex ultrasound and magnetic resonance imaging of the supra-aortic arches in patients with non recurrent inferior laryngeal nerve: a comparative study. G Chir 2011;32:245-50. [PubMed]
- Yetisir F, Salman AE, Çiftçi B, et al. Efficacy of ultrasonography in identification of non-recurrent laryngeal nerve. Int J Surg 2012;10:506-9. [Crossref] [PubMed]
- Satoh S, Tachibana S, Yokoi T, et al. Preoperative diagnosis of nonrecurrent inferior laryngeal nerve--usefulness of CT and ultrasonography. Nihon Jibiinkoka Gakkai Kaiho 2013;116:793-801. [Crossref] [PubMed]
- Wang Z, Zhang H, Zhang P, et al. Preoperative diagnosis and intraoperative protection of nonrecurrent laryngeal nerve: a review of 5 cases. Med Sci Monit 2014;20:233-7. [Crossref] [PubMed]
- Yang J, Yan SP, Gong YP, et al. The value of chest X-ray and cervical vascular ultrasound in predicting the presence of non-recurrent laryngeal nerves. Sichuan Da Xue Xue Bao Yi Xue Ban 2014;45:1036-9. [PubMed]
- Iacobone M, Citton M, Pagura G, et al. Increased and safer detection of nonrecurrent inferior laryngeal nerve after preoperative ultrasonography. Laryngoscope 2015;125:1743-7. [Crossref] [PubMed]
- Bayford D. An account of a singular case of obstructed deglutition. Mem Med Soc Lond 1789;2:275-86.
- Arkin A. Double aortic arch with total persistence of the right and isthmus stenosis of the left arch. A new clinical and x-ray picture. Report of 6 cases in adults. Am Heart J 1936;11:444-74. [Crossref]
- Stedman GW. A singular distribution of the nerves and arteries of the neck and the top of the thorax. Edinb Med Surg J 1823;19:564-5.
- De Luca L, Bergman JJ, Tytgat GN, et al. EUS imaging of the arteria lusoria: case series and review. Gastrointest Endosc 2000;52:670-3. [Crossref] [PubMed]
- Stewart GR, Mountain JC, Colcock BP. Non-recurrent laryngeal nerve. Br J Surg 1972;59:379-81. [Crossref] [PubMed]
- Hong KH, Park HT, Yang YS. Characteristic travelling patterns of non-recurrent laryngeal nerves. J Laryngol Otol 2014;128:534-9. [Crossref] [PubMed]
- Obaid T, Kulkarni N, Pezzi TA, et al. Coexisting right nonrecurrent and right recurrent inferior laryngeal nerves: a rare and controversial entity: report of a case and review of the literature. Surg Today 2014;44:2392-6. [Crossref] [PubMed]
- Maranillo E, Vazquez T, Quer M, et al. Potential structures that could be confused with a nonrecurrent inferior laryngeal nerve: an anatomic study. Laryngoscope 2008;118:56-60. [Crossref] [PubMed]
- Raffaelli M, Iacobone M, Henry JF. The "false" nonrecurrent inferior laryngeal nerve. Surgery 2000;128:1082-7. [Crossref] [PubMed]
- Iacobone M, Viel G, Zanella S, et al. The usefulness of preoperative ultrasonographic identification of nonrecurrent inferior laryngeal nerve in neck surgery. Langenbecks Arch Surg 2008;393:633-8. [Crossref] [PubMed]
- Kamani D, Potenza AS, Cernea CR, et al. The nonrecurrent laryngeal nerve: anatomic and electrophysiologic algorithm for reliable identification. Laryngoscope 2015;125:503-8. [Crossref] [PubMed]
- Branscom JJ, Austin JH. Aberrant right subclavian artery. Findings seen on plain chest roentgenograms. Am J Roentgenol Radium Ther Nucl Med 1973;119:539-42. [Crossref] [PubMed]
- Yusuf TE, Levy MJ, Wiersema MJ, et al. Utility of endoscopic ultrasound in the diagnosis of aberrant right subclavian artery. J Gastroenterol Hepatol 2007;22:1717-21. [Crossref] [PubMed]
- Katz AD, Nemiroff P. Anastamoses and bifurcations of the recurrent laryngeal nerve--report of 1177 nerves visualized. Am Surg 1993;59:188-91. [PubMed]