Circumcision with Glubran® 2 in children: experience of Italian Center
Introduction
Circumcision (from the Latin circum, “around” and caedere, “cut”) is one of the most common surgical procedures in the world (1). The circumcision can be performed for religious/cultural or medical reasons. Hemorrhage and infection are the most common complications of circumcision, followed by wound dehiscence, recurrent phimosis, preputial adhesions, trauma to the glans, and an ugly scar. Classical circumcision is performed using a standard technique with sutures for the approximation of the skin edges (2,3). However, since some years a tissue adhesive as N-butyl-2-cyanoacrylate (NBCA) plus methacryloxysulfolane (MS) (Glubran® 2) is used in many centers to circumcise children (4,5). The aim of our study was to compare two different methods for perform circumcision in children. The implication for practice was the understanding if there were differences between these approaches related to patient’s and parents benefits to manage this condition and benefits for surgeon and hospital in term of saving money and time.
Methods
Design/setting
This is a randomized, single-blind one-center study. It was conducted at the Department of Paediatric Surgery of Siena. Data were collected between March 2011 and December 2012.
Study’s population involved all patients who required circumcision. The enrollment of patients was done in the urology outpatient clinic. Parents were informed about the study and its objectives and their consent was obtained. After their decision to participate in this study, the child was placed in a computerized database. This database was used for recording and processing the data. It created two randomizes groups: group one which involved patients who underwent circumcision using sutures and group two, which involved patients who underwent circumcision using surgical glue (Glubran® 2). Patient did not know the kind of surgery before it.
Two exclusion criteria were used: the redo-circumcision and the allergy or hyper-sensibility to cyanoacrylate (main component of glue).
Operative techniques
The circumcision was performed using a sleeve technique. All patients received standard general anesthesia and additional local anaesthesia (dorsal penile block or ring block at the penile base with 2.5 mg/kg of 0.25% bupivacaine or 5 mg/kg of 1% lidocaine) to provide intraoperative anesthesia and postoperative analgesia. Short-term antibiotic therapy was dispensed after anesthesia induction. A postoperative dressing was used only for patients of group 1. It was a gauze around penis with anesthetic ointment (lidocaine).
Circumcision with sutures: patient was placed in supine position. The foreskin was retracted to expose the glands and the frenulum was not incised. Foreskin was pulled up carefully and it was excised with knife or bipolar.
Bleeding vessels were carefully cauterized. Mucosa was excised with unipolar or bipolar until about 1 cm from coronal sulcus. Dorsal and ventral interrupted sutures 5/0 (Vicryl Rapide) were placed circumferentially. We used a mean of 10 or 12 sutures. Circumcision with tissue glue (Glubran® 2): the first part of procedure was the same of circumcision with sutures. After cutting of foreskin, the mucosa was juxtaposed to skin with two forceps and the glue was applied circumferentially manually to create a thin film along the coronal sulcus.
Outcomes-measurements
Three outcomes were measured in three different moments and with differences scales.
The first outcome was the operating time. It was evaluated as < or >20 minutes and it was calculated at T0, during surgery.
The second outcome was the postoperative pain. It was evaluated with Faces Pain Scale-Revised (FPS-R) (6). Children were asked to indicate the face, which showed how much pain they had after surgery at home. The faces were six and they showed more and more pain from left to right. Each face was equivalent of numeric score 0, 2, 4, 6, 8, or 10 from left to right, so ‘0’ was ‘no pain’ and ‘10’ was ‘very much pain’. A score of < or =2 was considered optimal while a score of >2 suboptimal. It was calculated at T1, after 2 weeks from surgery. The evaluation was related to pain that they had during 3 days after surgery at home. We did not include the early postoperative pain evaluation, because many factors (anaesthetic effects, parent’s anxiety, psychological involvement) are involved to determine the postoperative reaction of patients. So we think that the results could be altered.
The third outcome was the assessment of cosmetic. It was performed using a modified Hollander wound evaluation scale (WES) (7,8). This parameter was evaluated at 2 weeks after surgery (T1) and 4 weeks after surgery (T2). The score was assigned and validated by a surgeon aware of the study but external to it. The wound score addressed six clinical variables: absence of step off, contour irregularities, wound margin separation >2 mm, edge inversion, excessive distortion, and overall cosmetic appearance. Each of these categories was graded on a 0- or l-point scale. A total cosmetic score was derived by the addition of the scores of the six categorical variables. A score of 6 was considered optimal, while a score of < or =5 suboptimal.
Statistical analysis
Comparisons between groups for the first outcome were performed using t-test; for second and third outcomes were performed using the Fisher’s exact test.
Ethical considerations
Ethics Committee Approval was informed but it was no necessary to perform the study, because Glubran was a medical product already employed in the hospital who granted permission for its use. Furthermore, this is a descriptive study, so the medical director’s of the hospital approval was enough. Informed consent form, however, was obtained from children’s parents before each procedure. We performed the study without external founds.
Results
We enrolled 239 patients. Nine of them were excluded: 2 for redo-circumcision and 7 for suspicion of hyper-sensibility to cyanoacrylate (it was obtained during the preoperative medical history). Two hundred and thirty were included and they were randomly divided in two groups: group 1—suture group involved 131 children, and group 2—glue group involved 99 patients.
One hundred and thirty eight (60%) of 230 underwent religious/cultural circumcision (76 group 1 and 62 group 2).
Ninety two patients (40%) underwent medical circumcision. The principal indications were a true pathological phimosis caused by the chronic cicatrising skin condition balanitis xerotica obliterans (BXO) (7 pts), ‘phimosis’ and recurrent balanoposthitis (46 pts), ‘phimosis’ and recurrent UTIs (35 pts) and acute urinary retention (4 pts).
The mean age of surgery was 6 years (1–18 years) in the group 1 and 5 years (1–13 years) in the group 2.
Only two surgeons performed all procedures. Another surgeon, aware of study, collected data and completed the database.
Operative techniques
No intraoperative or postoperative complications there were.
The in-patients stay was of 1 day.
Clinical outcomes
Operative time was <20 minutes in 38% of procedures in the group 1 and 80.8% in the group 2. The mean of duration of surgery in the suture group was 25.1 min (range, 15–45 min) rather 13.1 min (range, 10–25 min) in the glue group (Figure 1A). The T value is 0.290583. The P value is 0.392907. The result was not significant at P<0.05.
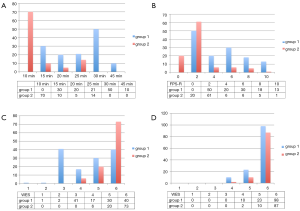
Postoperative pain evaluation showed: 50 (38.2%) patients of group 1 with optimal score, 81 (81.8%) with suboptimal score. A total of 81 (81.8%) of group 2 with optimal score and 18 (18.2%) with suboptimal (Figure 1B).
The two-tailed P value was less than 0.0001. The association between rows (groups) and columns (outcomes) was considered to be extremely statistically significant.
Early cosmetic evaluation (T1) showed: group 1, 40 (30.5%) with optimal score and 91 (69.5%) with suboptimal score. Group 2, 73 (73.7%) with optimal score and 26 (26.3%) with suboptimal score (Figure 1C). The two-tailed P value was less than 0.0001. The association between rows (groups) and columns (outcomes) was considered to be extremely statistically significant.
Late cosmetic evaluation (T2) showed: group 1, 98 (74.8%) with optimal score and 33 (25.2%) with suboptimal score. Group 2, 87 (87.8%) with optimal score and 12 (12.2%) with suboptimal score (Figure 1D). The two-tailed P value equalled 0.0181. The association between rows (groups) and columns (outcomes) was considered to be statistically significant.
Second and third outcomes were statistically significant. The first outcome was not statistically significant but two groups had a clear different operative time.
Results are showed in Figure 1A-D as graphics.
Discussion
Despite it is known the wide prevalence of circumcision for religious and medical reasons in children, it remains a controversial practice in paediatric age. To date, there is no described the gold standard technique. However among several possibilities one of last option is the use of tissue glue (Glubran® 2). It is a synthetic tissue adhesive, with haemostatic, adhesive, sealer and bacteriostatic properties. Since more than ten years it is used, in Italy and abroad, in many interventions of various types, both in traditional and laparoscopic surgery (cardiovascular, thoracic, vascular, and abdominal surgery) and in interventional radiology (4-6).
It is a synthetic surgical glue consisting of NBCA plus MS (NBCA + MS) modified by the addition of a monomer which allows obtaining an exothermic polymerization reaction at around 45 °C with a slightly higher polymerization time than other cyanoacrylate glues (4,5). On contact with biological tissues in a moist environment, glue rapidly polymerizes to create a thin elastic film of high tensile strength, which guarantees firm adherence of tissues. The film easily tailors to the planes and tissues of application, is totally water resistant, and is not impaired by the presence of blood or organic fluids. When correctly applied, the glue begins solidification within 1 or 2 second and completes the process within 60 or 90 seconds. The glue reaches its maximum mechanical strength upon completion of this reaction. The product is 1, 0.5 and 0.25 ml single dose. It is ready for use (it needs no preparation) and has to be stored at temperatures between 0 and +4 °C (9-12).
We started to use glue for circumcision about 2 years ago. We designed this prospective study to analyze our data, compare them with literature and share our experience with this product.
We report 99 patients who underwent circumcision with Glubran® 2 in comparison with a group of children circumcised with sutures. We measured three outcomes, which, even if not all statistically significant, allowed us to draw any conclusions about the use of glue in circumcision. The first outcome that we considered was the operating time. The choice of this point was done especially to understand if the use of one of two techniques of circumcision could give practical advantages to surgeons. It is clear, indeed, that a faster surgery allows to include more patients in a same list and to reduce the waiting list. It should be also considered that a faster surgery requires less anaesthesia and this is a benefit for patients. This parameter was greatly reduced during Glubran® 2 procedure indeed the mean of duration of surgery in the suture group was 25.1 min (range, 15–45 min) rather 13.1 min (range, 10–25 min) in the glue group. However the statistical evaluation showed no significance. It is important underline that even if the application of glue is simple, the learning curve is however important and the personal ability could be a bias. For this reason, indeed, we assigned only two surgeons to perform glue application. The second outcome that we evaluated was the postoperative pain at home (in 3 days after surgery). It is known indeed that the management of pain in child is often a challenge for parents and doctors. The evaluation of pain was done with the FPS-R (1). It is a self-report measure of pain intensity developed for children. It is easy to administer and requires no equipment except for the photocopied faces. It is particularly recommended for use with younger children. We decided to use this scale because the median age of our patients was 5.5 years. Fifty (38.2%) patients of suture group have ticked the first two faces of scale versus eighty one (81.8%) of group 2.
The statistical comparison was statistically significant, these data show that patients underwent glue circumcision had less pain after surgery. Even if outcomes such as pain and time were very important, final cosmetic result was the most important outcome, which we evaluated. The aspect of this part of the body, indeed, has a heavy psychological impact for child and parents. The assessment of cosmesis was done with a previously validated WES, which has been demonstrated to be reliable and valid. The statistic analysis showed significance. The main difference between two groups seemed related to the precocity to good cosmesis. Indeed, at T1 only 30.5% of patients circumcised with sutures had an optimal score versus 73.7% of them circumcised with glue (Figure 2). The final cosmesis, measured after 4 weeks from surgery, did not seem different because 74.8% of suture group and 87.8% of glue group had an optimal score. Based on these results, it is clear that the long-term results are not influenced by technique but the glue gives a good aesthetic result more quickly. This means that patient has a less psychological impact and he can back to his normal life without any restrictions.
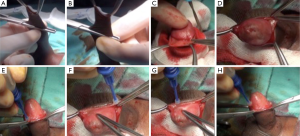
About surgical aspect, we want cite that, in addition to all outcomes which we measured and discussed above, unlike other studies, we describe a different method for circumcision with Glubran® 2. Edges of skin and mucosa were approximated only with glue without applying sutures. In Figure 3 there are showed main steps of glue application. This allowed to not use any dressing at the end of procedure. So, patients had not a psychological trauma or postoperative pain during the removal dressing, they used underwear in the early postoperative period and they took baths according to their usual routines (after 48 hours) after discharge. All of these are other advantages of glue technique. Finally we believe that the bacteriostatic properties of Glubran® 2 can reduce risks of infection which is the most common complication of circumcision. In our series we did not have infection, maybe because of all our patients had antibiotic therapy during surgery.
The use of tissue glue for circumcision in children is already described in literature from several years. We reviewed these data and compared whit our results. Ozkan et al. (13) suggested that tissue glue approximation in circumcision is a feasible alternative especially because the operating time is shorter and a cosmetic result was superior. We can confirm all of these even if our results about operative time are no statistically significant.
Subramaniam and Jacobsen (14) described that circumcision with cyanoacrylate caused less pain and pain of a shorter duration than that with standard sutured closure. We are agreed with these authors and our data confirm these conclusions. Elmore et al. (3) reported 267 boys, who underwent circumcision with two thin layers of 2-octyl-cyanoacrylate. They suggested that suture less circumcision closure using glue tissue is a safe, fast, and cosmetically appealing alternative to standard interrupted suture approximation. In our opinion, one layer is enough for wound approximation.
Conclusions
Based on our results we can conclude that, glue (Glubran® 2) application is an excellent alternative to circumcision in paediatric age. In our opinion circumcision with this technique has got many advantages. Firstly, it is faster than suture circumcision, so anaesthetic time is reduced for child and more patients can be operated in the same time. Secondly, child has got less postoperative pain and the parent’s management is simpler. Finally, cosmetic result is better and earlier than suture circumcision. However, it is important a good learning curve to ensure a right application of glue and good results especially in term of cosmetic.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics Committee Approval was informed but it was no necessary to perform the study, because Glubran was a medical product already employed in the hospital who granted permission for its use. Furthermore, this is a descriptive study, so the medical director’s of the hospital approval was enough. Informed consent form, however, was obtained from children’s parents before each procedure. We performed the study without external founds.
References
- Ozturk H, Karaaslan K, Kocoglu H. HAYRETTIN Use of Glubran 2 Surgical Glue in Circumcision Results in a Comfortable Postoperative Period. Adv Clin Exp Med 2009;18:381-4.
- Weiss HA, Larke N, Halperin D, et al. Complications of circumcision in male neonates, infants and children: a systematic review. BMC Urol 2010;10:2. [Crossref] [PubMed]
- Elmore JM, Smith EA, Kirsch AJ. Sutureless circumcision using 2-octyl cyanoacrylate (Dermabond): appraisal after 18-month experience. Urology 2007;70:803-6. [Crossref] [PubMed]
- Kull S, Martinelli I, Briganti E, et al. Glubran2 surgical glue: in vitro evaluation of adhesive and mechanical properties. J Surg Res 2009;157:e15-21. [Crossref] [PubMed]
- Leonardi M, Barbara C, Simonetti L, et al. Glubran 2: a new acrylic glue for neuroradiological endovascular use. Experimental study on animals. Interv Neuroradiol 2002;8:245-50. [PubMed]
- Hicks CL, von Baeyer CL, Spafford PA, et al. The Faces Pain Scale-Revised: toward a common metric in pediatric pain measurement. Pain 2001;93:173-83. [Crossref] [PubMed]
- Hollander JE, Singer AJ, Valentine S, et al. Wound registry: development and validation. Ann Emerg Med 1995;25:675-85. [Crossref] [PubMed]
- Quinn JV, Drzewiecki AE, Stiell IG, et al. Appearance scales to measure cosmetic outcomes of healed lacerations. Am J Emerg Med 1995;13:229-31. [Crossref] [PubMed]
- Montanaro L, Arciola CR, Cenni E, et al. Cytotoxicity, blood compatibility and antimicrobial activity of two cyanoacrylate glues for surgical use. Biomaterials 2001;22:59-66. [Crossref] [PubMed]
- Barillari P, Basso L, Larcinese A, et al. Cyanoacrylate glue in the treatment of ano-rectal fistulas. Int J Colorectal Dis 2006;21:791-4. [Crossref] [PubMed]
- Dickneite G, Metzner H, Pfeifer T, et al. A comparison of fibrin sealants in relation to their in vitro and in vivo properties. Thromb Res 2003;112:73-82. [Crossref] [PubMed]
- Arunachalam P, King PA, Orford J. A prospective comparison of tissue glue versus sutures for circumcision. Pediatr Surg Int 2003;19:18-9. [PubMed]
- Ozkan KU, Gonen M, Sahinkanat T, et al. Wound approximation with tissue glue in circumcision. Int J Urol 2005;12:374-7. [Crossref] [PubMed]
- Subramaniam R, Jacobsen AS. Sutureless circumcision: a prospective randomised controlled study. Pediatr Surg Int 2004;20:783-5. [Crossref] [PubMed]