Factors associated with patients in the Scottish Highlands who chose mastectomy when suitable for breast conservation
Introduction
Both breast conservation surgery (BCS) with adjuvant radiotherapy and mastectomy offer equivalent oncological outcomes for women with newly diagnosed breast cancer, yet some women offered BCS choose to undergo mastectomy (1,2). The issue of variation in mastectomy rates has been highlighted within the UK (3). Analysis of the Trent Breast Screening Programme database [1997–2003] found statistically significant variations in the surgical management of early stage breast cancer with regards to mastectomy rates. The authors conclude that the variation in mastectomy rates within the programme cannot be accounted for by case-mix alone and recommend further research to investigate the potential factors influencing the type of surgery in breast cancer. Similar variation has been highlighted in the United States (4,5).
A range of factors have been found to be associated with women choosing mastectomy rather than BCS including larger tumour size (6), residing in a rural or remote setting (4,7,8) and wish to avoid radiotherapy (9-14). The Highland Breast Centre provides both screening and symptomatic breast services to the Highlands and Western Isles of Scotland, a population of approximately 310,000 living within approximately 40% of the land mass of the country. Given that the unit provides services to both urban and rural populations it is well placed to assess if the previously found factors associated with patients choosing mastectomy are replicated in the Scottish setting.
The aim of this study was to assess which pre-operative tumour characteristics, and geographical factors are associated with a patient’s decision to undergo mastectomy when suitable for BCS.
Methods
Patients
A retrospective analysis of the electronically stored minutes from the multi-disciplinary team meetings between January 2011 and December 2013 was carried out to identify all patients who underwent mastectomy during this time and case note review identified those who chose mastectomy for invasive carcinoma when BCS would have been appropriate. This assessment was made from careful reading of the pre-operative clinic letters by two members of the research team (RS/MR). Patients were included for analysis if the clinic correspondence clearly highlighted that BCS had been offered as being a viable option. Patients who underwent immediate breast reconstruction were also included. Patients undergoing bilateral mastectomy were excluded. All patients undergoing BCS during the same time period were included for comparison. Patients were deemed suitable for BCS when the multidisciplinary team felt that clear oncological resection of the tumour would not compromise the final cosmetic result. At pre-operative consultation the operating surgeon discussed all options and detailed the oncological equivalence of BCS and radiotherapy compared to mastectomy.
Methods
Pre-operative tumour characteristics for all patients (size on imaging, grade, pre-operative axillary nodal staging and tumour sub-type) were retrieved from the online results system (SCI Store v8.3, NHS National Services Scotland). All patients underwent axillary ultrasound at diagnostic assessment and guided core biopsy performed in the presence of abnormal nodes. Axillary staging was defined as positive when guided core biopsy was positive for metastatic disease at pathological assessment. Pathological assessment of core biopsies was carried out according to national standards (15).
The distance from the patient’s home to the treatment centre was calculated using Google Maps© (Map data 2014 Google, Mountain View, California, USA) using the shortest distance. The need for either air or ferry transportation was also noted. The degree of socio-economic deprivation was assessed using the Scottish Index of Multiple Deprivation Score (SIMD) 2012 data (16).
To further investigate the personal reasons for choosing mastectomy rather than BCS a questionnaire was sent to those patients (Supplementary). This questionnaire explored the individual’s reasons for their choice and their feelings with regard to their decision. For each question, patients were able to choose more than one answer. A free text box was provided after each question for other comments.
Local research and development and ethical approval was obtained (14/WS/1151).
Statistical analysis
Statistical analysis was undertaken using SPSS 22.0 software (SPSS Inc., Chicago, IL, USA). Pre-operative tumour characteristics and geographic data were compared using the Pearson’s Chi-squared test. A P value of <0.05 was considered statistically significant.
Results
Pre-operative tumour characteristics and geographic details
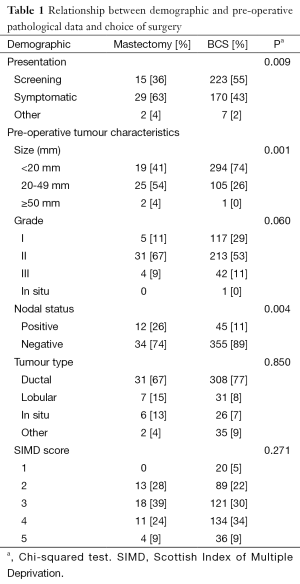
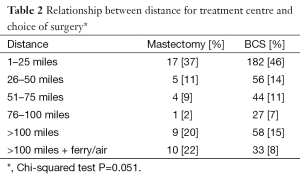
A total of 446 patients were identified as being suitable for BCS of which 46 (11%) chose to undergo mastectomy. The median ages were 66 (range, 44–86) and 62 (range, 33–87) years for the mastectomy and BCS groups respectively. Relationships between demographic and pre-operative pathological data for the two groups are shown in Table 1. Women choosing to undergo mastectomy were more likely to have presented symptomatically (P=0.09), have a tumour larger than 20 mm on diagnostic imaging (P=0.01) and have positive pre-operative axillary lymph node staging (P=0.04). There was no significant correlation found with SIMD score. There was a trend for patients living remotely from the treatment centre to choose mastectomy but this failed to reach statistical significance (Table 2).
Full table
Full table
Questionnaire
Of the 46 patients choosing mastectomy, 41 were alive and sent a questionnaire and 27 (66%) provided a reply.
Reasons for choosing mastectomy over BCS
A better long-term outcome and peace of mind were the most common reasons stated by 18 (44%) and 14 (34%) women respectively. The wish to avoid radiotherapy was a factor for 11 (27%) women. Other issues included family reasons, influence of others, a co-morbidity that would lead to transport difficulties that may be incurred with repeat trips to the hospital for further surgery or radiotherapy.
Avoidance of radiotherapy
Of those 11 women who highlighted wish to avoid radiotherapy as a factor for choosing mastectomy, the requirement to stay away from home was an influence for 7 (64%) women and distance was an influence for 5 (45%) women. Potential costs of travelling or staying close to the treatment centre, or being a carer were an issue for 5 women (45%). Two (18%) women cited a wish to avoid the effects of radiotherapy and one wished to avoid the extra burden of treatment.
Happiness with choice
All 27 (100%) women felt happy with their choice of mastectomy over BCS. Free-text comments included the common theme of “peace of mind” as with the breast removed they felt the cancer could not recur at on the ipsilateral side. In a number of cases, the women commented that the tumour was upgraded on final pathology or that further tumours were found in that breast and this had positively reinforced their choice for mastectomy.
Additional resources
Most women (16, 59%) felt they wouldn’t have benefited from receiving anything additional during the informed consent process. A total of 7 (26%) women indicated that meeting women who had gone through a similar decision-making process would have been helpful. Additionally, information regarding accommodation facilities for the duration of radiotherapy would have been useful, along with assistance with arranging care and information on claiming travel and accommodation expenses.
Discussion
The Scottish Intercollegiate Guidelines Network (SIGN) guideline for the treatment of primary invasive breast cancer recommends that women should be offered the option of BSC or mastectomy (17). Furthermore, the choice of surgery must be tailored to the individual patient, and they should be fully informed of the requirement for radiotherapy following BCS or further surgery should the margins be positive. Currently in Western Europe, 60–80% of new cancers are amenable to BCS (18). The rate of BCS has been suggested as a marker of quality of breast care centres, with a minimum standard of 70% of patients with invasive breast cancer and tumours not larger than 3 cm to undergo BCS, and an aim for 80% to be met by the European community (19). The position paper does mention other factors need to be considered such as patient preference. Taking this one step further, one national quality performance indicators (QPIs) for breast cancer care introduced across Scotland in 2012 is a target to treat 85% of patients with small breast cancers, <20 mm in diameter, by breast conservation whenever appropriate (20). This was updated in 2013 to include the caveat that tolerance within this target level accounts for the fact that BCS may not always be appropriate, particularly due to patient choice (21).
If the rate of BCS is to be used as a marker of care, it is important to understand what influences the decision making process for patients in order to provide best care. Patients should be able to make an informed choice, but with pressures on the surgeon to achieve targets, this choice may be jeopardised. If there are factors beyond the patients’ control, such as distance to travel for treatment, service redesign could be considered to mitigate these. Although distance from surgical treatment and radiotherapy centres have both been shown to influence mastectomy rates (4,7-14), this study was short of showing statistical significance The numbers in our study are small and reflect the small but scattered population of the Scottish Highlands and Islands, and sample size may have limited the ability to show statistical significance despite a trend that showed rurality influenced choice for mastectomy.
Unlike some studies, both the surgical treatment and radiotherapy take place at the central treatment centre for patient included in the current study. Therefore, regardless of surgical decision, patients have to travel the same distance for treatment, with those undergoing radiotherapy requiring to spend longer away from home. Just over a quarter of patients who responded to the questionnaire cited avoidance of radiotherapy as a factor and, of those women, over half felt travelling distance or a requirement to stay away from home to receive radiotherapy was an issue. Although not statistically significant, this is an issue for a subset of patients when it comes to making their decision, and should be considered by health boards when designing, or making decisions about the location of treatment centres.
This study has shown an association between established adverse tumour characteristics and decision to undergo mastectomy. These findings support the literature that has found tumour pathology is an influencing factor behind a patient’s decision for surgery, specifically larger tumour size, higher-grade tumours and positive axillary staging (3,6,7,22). Importantly, the published studies do not make it clear whether the tumour data relates to pre-operative or post-operative findings. In order to influence patient’s decision, the tumour characteristics from diagnosis are those that are important. Given that the majority of patients cited a perceived better outcome with mastectomy it may be possible that a patients choice is influenced by the pre-operative information given. At the time of informed consent, the surgeons put forward the evidence that there is no difference in outcome between mastectomy and BCS, highlighting the importance of radiotherapy as part of this treatment choice. If despite this information the patient is resolute in their decision then follow up contact pre-operatively to ensure that they remain so may be prudent. Previous studies have identified that patients feel safer after mastectomy, and that fear of recurrence and perceived survival benefit are primary motivators for choosing a mastectomy over BCS (23,24), and fear or recurrence remains an issue in the long-term, which is a challenge (25,26). Given these beliefs it may be that the communication of adverse pre-operative pathological features may influence the patient’s decision to pursue mastectomy. Improvement in the way we deliver information to our patients regarding the surgical options is one aspect that needs to be considered. Some of the patients here felt that speaking to a patient who had to make a similar decision would have been helpful, and this may be something than could be accommodated in the future.
The effect of deprivation on mastectomy rates was previously looked at by another Scottish centre in 2005 (27). Although patients from deprived areas were more likely to undergo mastectomy, this was felt to be due to these patients presenting symptomatically or with larger tumours, rather than deprivation being a factor itself. Deprivation was calculated using the Carstairs index, but since then the SIMD score has been developed and allows smaller pockets of deprivation to be identified. Similar to Henley et al. (27), there was no correlation between deprivation and type of surgery in our current study. However, despite an updated scoring system, there are still limitations, particularly when studying rural populations as the postcodes cover large areas with low numbers of residents, and are less effective at correlating deprivation on an individual basis, making firm conclusions hard to make.
Conclusions
Supporting patients in making a decision regarding surgery for breast cancer is vital. This study has shown that although not significant, distance to travel for treatment does play a part in a subset of patients, and not just those who live the furthest from the treatment centre. Adverse pre-operative tumour characteristics are associated with the choice of mastectomy, however further studies are needed to establish if this information does indeed influence the patient’s choice. The perceived oncological benefit by patients does suggest that this may be the case. This study raises the importance of detailed individualised treatment taking into account both the pathological data and the patient’s personal circumstances.
Acknowledgements
The authors would like to thank Mr Stuart Suttie of the Department of Vascular Surgery, Ninewells Hospital, Dundee, UK for his assistance with statistical analysis.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Local research and development and ethical approval was obtained (14/WS/1151).
Supplementary
Questionnaire
1. What were your reasons for choosing mastectomy over wide-local excision and radiotherapy? Tick all that apply.
- Wish to avoid radiotherapy
- Peace of mind
- Family reasons
- Previous mastectomy on the other side
- Feel this provides a better long-term outcome
- Influenced by someone you know who has been through the same experience
- Other
If other please state the reason/s: .............................................................................................................................................................................................................................................
2. If you chose “wish to avoid radiotherapy” above, which of the following were behind this decision?Tick all that apply.
- Distance to travel from home to radiotherapy centre daily
- Requirement to stay away from home for the 3 week duration of radiotherapy
- Potential cost involved with travelling or accommodation
- Main carer for someone and felt could not commit to 3 weeks of radiotherapy
- Other
If other please state the reason/s: ........................................................................................................................................................................................................................................................................
3. Reflecting on your decision now, are you happy with the choice you made to undergo mastectomy?
- Yes
- No
Why?
...................................................................................................................................................................................................................................................................................................
4. Which of the following, if offered during your discussions regarding surgery, would have been useful to help with your decision? Tick all that apply.
- Information regarding patient +/- family accommodation facilities at Raigmore hospital for duration of radiotherapy treatment
- Opportunity to speak to other patients who had undergone breast surgery and had a similar decision to make
- Assistance with arranging care for family/relatives
- Information regarding how to claim money for travel +/- accommodation
- None of the above
- Other
If other please state the reason/s: ........................................................................................................................................................................................................................................................................
5. Please make any other comments
....................................................................................................................................................................................................................................................................................................................................................
---- End of questionnaire ---
References
- Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233-41. [Crossref] [PubMed]
- Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227-32. [Crossref] [PubMed]
- Caldon LJ, Walters SJ, Reed JA, et al. Case-mix fails to explain variation in mastectomy rates: management of screen-detected breast cancer in a UK region 1997-2003. Br J Cancer 2005;92:55-9. [Crossref] [PubMed]
- Dragun AE, Huang B, Tucker TC, et al. Increasing mastectomy rates among all age groups for early stage breast cancer: a 10-year study of surgical choice. Breast J 2012;18:318-25. [Crossref] [PubMed]
- Adkisson CD, Bagaria SP, Parker AS, et al. Which eligible breast conservation patients choose mastectomy in the setting of newly diagnosed breast cancer? Ann Surg Oncol 2012;19:1129-36. [Crossref] [PubMed]
- Roder D, Zorbas H, Kollias J, et al. Factors predictive of treatment by Australian breast surgeons of invasive female breast cancer by mastectomy rather than breast conserving surgery. Asian Pac J Cancer Prev 2013;14:539-45. [Crossref] [PubMed]
- Taylor R, Stubbs JM, Langlands AO, et al. Predictors of Mastectomy for Women with Breast Cancer in the Greater Western Region of Sydney. Breast J 1999;5:116-21. [Crossref] [PubMed]
- Dragun AE, Pan J, Riley EC, et al. Increasing use of elective mastectomy and contralateral prophylactic surgery among breast conservation candidates: a 14-year report from a comprehensive cancer center. Am J Clin Oncol 2013;36:375-80. [Crossref] [PubMed]
- Voti L, Richardson LC, Reis IM, et al. Treatment of local breast carcinoma in Florida: the role of the distance to radiation therapy facilities. Cancer 2006;106:201-7. [Crossref] [PubMed]
- Meden T, St John-Larkin C, Hermes D, et al. MSJAMA. Relationship between travel distance and utilization of breast cancer treatment in rural northern Michigan. JAMA 2002;287:111. [Crossref] [PubMed]
- Jacobs LK, Kelley KA, Rosson GD, et al. Disparities in urban and rural mastectomy populations: the effects of patient- and county-level factors on likelihood of receipt of mastectomy. Ann Surg Oncol 2008;15:2644-52. [Crossref] [PubMed]
- Athas WF, Adams-Cameron M, Hunt WC, et al. Travel distance to radiation therapy and receipt of radiotherapy following breast-conserving surgery. J Natl Cancer Inst 2000;92:269-71. [Crossref] [PubMed]
- Schroen AT, Brenin DR, Kelly MD, et al. Impact of patient distance to radiation therapy on mastectomy use in early-stage breast cancer patients. J Clin Oncol 2005;23:7074-80. [Crossref] [PubMed]
- Boscoe FP, Johnson CJ, Henry KA, et al. Geographic proximity to treatment for early stage breast cancer and likelihood of mastectomy. Breast 2011;20:324-8. [Crossref] [PubMed]
- NHSBSP. Pathology Reporting Of Breast Disease. 2005. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/465530/nhsbsp58-high-resolution.pdf
- The Scottish Government. Scottish Index of Multiple Deprivation 2012 [cited 2015 Nov 2]. Available online: http://simd.scotland.gov.uk/publication-2012/
- Scottish Intercollegiate Guidelines Network (SIGN). Treatment of primary breast cancer. Edinburgh: SIGN; 2013. (SIGN publication no. 134). [September 2013]. Available online: http://www.sign.ac.uk
- Senkus E, Kyriakides S, Ohno S, et al. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26 Suppl 5:v8-30. [Crossref] [PubMed]
- Del Turco MR, Ponti A, Bick U, et al. Quality indicators in breast cancer care. Eur J Cancer 2010;46:2344-56. [Crossref] [PubMed]
- ISD Scotland. Breast cancer quality performance indicators. 2014. Available online: http://www.isdscotland.org/Health-Topics/Quality-Indicators/Publications/2014-04-29/2014-04-29-BreastQPI-Report.pdf
- Healthcare Improvement Scotland. Cancer Quality Performance Indicators (QPIs). [cited 2015 Oct 29]. Available online: http://www.healthcareimprovementscotland.org/our_work/cancer_care_improvement/cancer_qpis/quality_performance_indicators.aspx
- Rippy EE, Ainsworth R, Sathananthan D, et al. Influences on decision for mastectomy in patients eligible for breast conserving surgery. Breast 2014;23:273-8. [Crossref] [PubMed]
- Fisher CS, Martin-Dunlap T, Ruppel MB, et al. Fear of recurrence and perceived survival benefit are primary motivators for choosing mastectomy over breast-conservation therapy regardless of age. Ann Surg Oncol 2012;19:3246-50. [Crossref] [PubMed]
- Kirby RM, Basit A, Manimaran N. Patient choice significantly affects mastectomy rates in the treatment of breast cancer. Int Semin Surg Oncol 2008;5:20. [Crossref] [PubMed]
- Koch L, Bertram H, Eberle A, et al. Fear of recurrence in long-term breast cancer survivors-still an issue. Results on prevalence, determinants, and the association with quality of life and depression from the cancer survivorship--a multi-regional population-based study. Psychooncology 2014;23:547-54. [Crossref] [PubMed]
- Janz NK, Leinberger RL, Zikmund-Fisher BJ, et al. Provider perspectives on presenting risk information and managing worry about recurrence among breast cancer survivors. Psychooncology 2015;24:592-600. [Crossref] [PubMed]
- Henley NC, Hole DJ, Kesson E, et al. Does deprivation affect breast cancer management? Br J Cancer 2005;92:631-3. [Crossref] [PubMed]


